My Miraculous Conception
How two infertility doctors, a team of nurses, an embryologist, an acupuncturist, my husband, and I made a baby.
I was 27 when I started trying to get pregnant. Two years in, a doctor told me that my eggs were no good (he didn’t know why) and that it was unlikely that I would ever get pregnant naturally. Still, my husband, Mike, and I kept trying for another year, exhausting every affordable DIY infertility treatment imaginable, from herbal and holistic to high-tech. We even ventured into old-wives-tale territory. Nothing worked. Throughout those years, the day my period arrived was the worst day of every month. Its arrival always felt like another nail in the coffin, another confirmation that my dream of being a mother was doomed.
After three long years of trying and much consideration, we decided to spend some of the money we’d saved for a house down payment on in-vitro fertilization. We had no idea what to expect. In February 2010, I started documenting my first—and as it turned out, my only—IVF cycle, in hopes of sharing the process with other women battling infertility. Ten months and $23,241 later (and five years after I first started trying to get pregnant), I gave birth to our daughter.
-
 Shawnee Barton.
Shawnee Barton.Stalled
Battling infertility feels like being stuck on the side of the road without a spare tire. My life stands frustratingly still while I watch other women’s lives whiz past.
I want to know why my body can’t make a baby, and I am willing to do whatever I need to do to get it fixed, which is how I ended up like this: lying on a gurney with a body full of needles.
-
 Shawnee Barton.
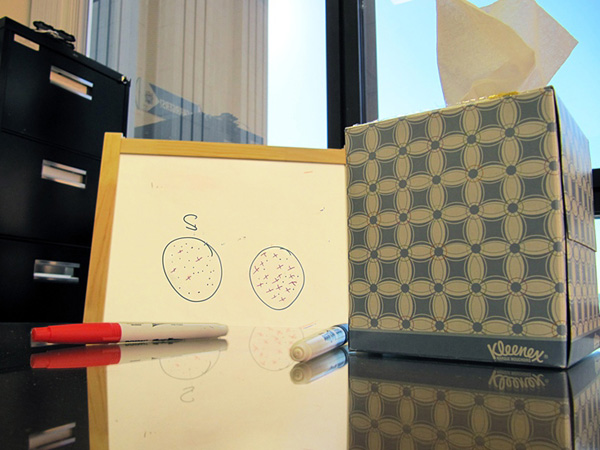
Shawnee Barton.Bad News
Our doctor blocks off time at the end of each week to deliver bad news to patients. As my husband, Mike, and I wait, a train of women and men emerge from his office deflated. When it’s our turn, he tells us that low levels of a hormone known as FSH indicate that my eggs are no better than those of a 40-year-old. Then, he draws a picture on his whiteboard repeating what he just said. “Thanks,” I say, “I got it.” Clenching my jaw allows me to hold myself together, but as soon as I get to the parking lot, I start heaving.
-
 Shawnee Barton.
Shawnee Barton.Not that Kind of Ultrasound
Cruelly, the same machine used to look at soon-to-be-born babies also illuminates infertility problems. Lately, this wand has been inside of me more than my husband. Each time, I reflexively look for a fetus on the screen, even though I know there isn’t one to see.
After three failed rounds of intrauterine insemination (IUI), in which my husband’s sperm was implanted in my uterus via catheter, we find a different doctor. The long string of letters following our new specialist’s name on the plaque outside his door make me feel confident in his abilities. Dr. Sanjay Agarwal, M.D., F.A.C.O.G., has a gentle demeanor. Unlike our previous doctor, he is optimistic about our chances of conceiving. He has creative ideas and he doesn’t own a whiteboard.
Dr. Agarwal tells us that because our issue is egg quality, IUIs are unlikely to significantly improve our chances of conceiving. Still, IUIs are roughly $17,000 less expensive per cycle than IVF, so we try two more cycles. After they both fail, we resign ourselves, and our savings account, to doing whatever it takes.
-
 Shawnee Barton.
Shawnee Barton.Drug Store
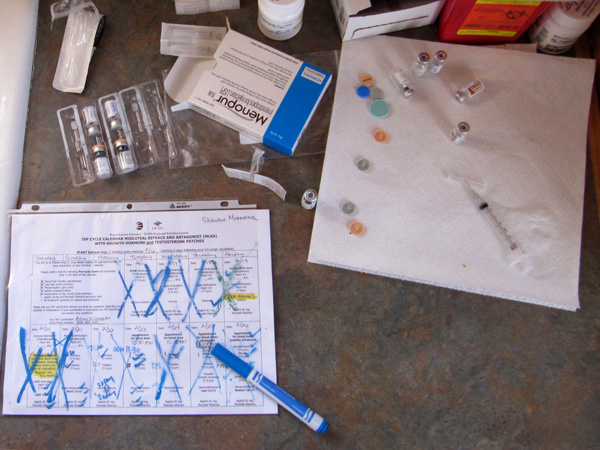
For the five IUIs, I bought leftover vials of an expensive drug called Follistim from other women who had either gotten pregnant or given up. But now that we’re turning to IVF, we’ve switched to the only insurance plan we can find that covers infertility-related prescriptions. Seeing the $5,000 worth of drugs needed for just one IVF cycle piled high on my kitchen table overwhelms me, and I think for the first time, “This can’t be good for my body,” but stopping doesn’t really feel like an option.
-
 Shawnee Barton.
Shawnee Barton.Nineteen Shots, Seven Patches, and 126 Pills
In all, the cycle includes 19 shots, seven patches, and 126 pills. I have two weeks of estrogen pills behind me. Those pills stopped my menstrual cycle, enabling my doctor to restart it on his clock. Today I begin taking shots. I am injecting 125 IUs of Follistim and 75 IUs of Menopur, a hormone extracted from the urine of postmenopausal women. Together, they will make my body do things nature never intended. Most women release one egg a month, but several days of these horomone injections will exponentially increase the number of eggs my body releases this month. I feel excited, nervous, and grateful all at once.
-
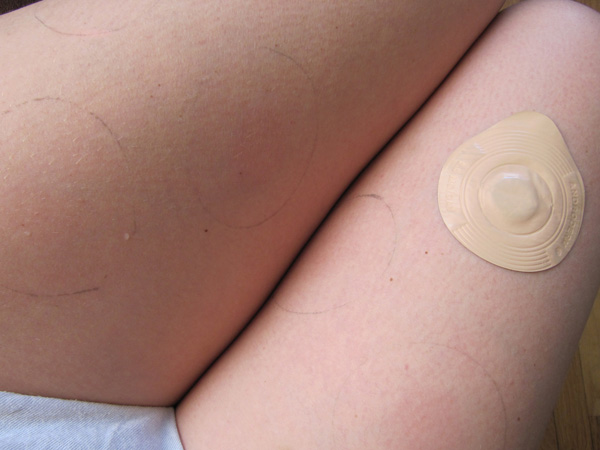
Good Eggs and Bad Eggs
Dr. Agarwal hopes that a relatively new strategy will improve my egg quality, which until now has been described to us as unfixable. Testosterone and human growth hormone steroids can magically turn a has-been ballplayer into a franchise slugger. Those same hormones may have the potential to turn old, bad eggs with thin outer linings into good ones, so he’s added them to the usual IVF cocktail.
The residue from the testosterone patches won’t come off with soap or even rubbing alcohol. Thankfully, it’s not swimsuit season.
-
Shawnee Barton.
The George Steinbrenner of Infertility
The baseball field outside the clinic’s exam room window calms me. I imagine myself as the George Steinbrenner of infertility, trying to create the deepest baby-making bench possible. We flew to Colorado to scout what many believe is the best clinic in the country, and we’ve already cut one doctor and one nurse from our roster. Now, we have two new doctors, a fantastic team of nurses, an embryologist, a psychologist, an acupuncturist, multiple books, and a sweet dog that snuggles with me when I lie in bed and cry my way through the toughest days.
-
Shawnee Barton.
A Good Man
There is no way to know beforehand if life’s big challenges will strengthen your relationship or pull it apart. But Mike is a good man, and never once have I felt like I was battling this alone. I need to be a mother, and if I had to, I would go through this by myself, as many women do. But while I could handle the process, I am not sure I could handle failure. I am pretty sure it would break me. Knowing that Mike and I will make it through this and find a way to build a happy family—with or without a biological baby—is an extraordinary comfort.
-
 Shawnee Barton.
Shawnee Barton.The Most Stressful Egg Hunt Ever
Halfway through the cycle: My meds take up just one shelf in the fridge now instead of two. Noticing the egg carton on the next shelf reminds me that I am getting ready for the most stressful egg hunt ever.
Since a woman’s eggs are too small to be seen on an ultrasound, doctors count follicles, the fluid-filled sacks the eggs grow inside, to see how well fertility medications are working. Today, Dr. Agarwal will look for follicles inside me. If he doesn’t find enough, we will have to start all over.
-
 Shawnee Barton.
Shawnee Barton.IVF on the Road
Traveling during an IVF cycle is nearly impossible. The constant clinic visits, the refrigerated medications, the shots at specific times all add intensity to the process and keep patients close to home. Tonight, though, a friend is having a birthday party that we don’t want to miss, so we load the car with flowers for her and a cooler full of medicine for me.
At the clinic yesterday, I learned that I have a good number of follicles. Not all of them are growing at the desired rate, but I am grateful that my doctor says we can move forward.
-
 Shawnee Barton.
Shawnee Barton.A Day in the Month
This calendar keeps track of my complicated medication schedule. I am immersed in the fertility process and have fallen behind on chores: returning calls, exercising, doing dishes. I can tell my body is reacting to the hormones. I recently noticed hair growing on my stomach, and I am getting excessively moody and sensitive. A week ago, my grandfather told me to not let the doctors turn me into “Octomom.” Today, his wife asks Mike if the hormones have turned me into “Dr. Jekyll and Mrs. Hyde.” She was half-joking, of course, but I’m not laughing.
She was half joking, of course, but I’m not laughing.
-

Needled
I am lucky. We have the money to try to make a baby. I think constantly about the women who don’t, women who want a child as much as I do. But even as I am grateful, I am at the end of my rope with the needles. My arms look like an addict’s. Each day, I go to the clinic, pay to park, and ride to the eighth floor so that a nurse can draw blood. But the more bruised my arms get, the harder it is for her to hit her target. Today, when she missed a fifth time, I started crying. Not because it hurt, but because I am exhausted and fed up with feeling like a pincushion.
-
 Shawnee Barton.
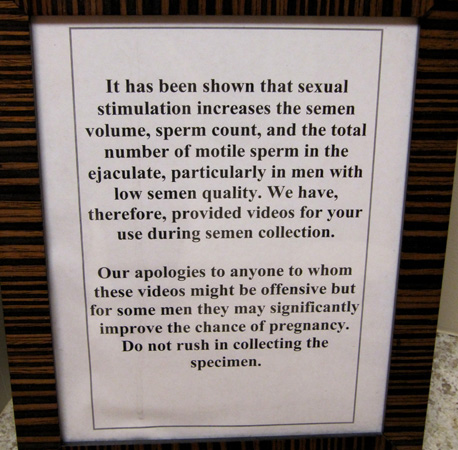
Shawnee Barton.Barely Legal or Cougar Hunt?
To remove 11 (eleven!) eggs of varying quality from my uterus this morning, it took pain meds, a doctor, nurses, a catheter, an ultrasound machine worth more than my house, a microscope, and an embryologist. Sperm retrieval is less high-tech. The toughest part of Mike’s physical contribution to this process was choosing between Barely Legal and Cougar Hunt. Afterward, the doctor comes in to tell us how fast and plentiful his sperm are. This should probably fill me with pride and hope, but instead, it makes me more aware of my inadequacies.
-
 Shawnee Barton.
Shawnee Barton.To the Petri Dishes
Minutes later, the embryologist implants one healthy sperm into each of the 11 freshly extracted miracle eggs. This process—Intra Cytoplasmic Sperm Injection, or ICSI—is now standard in most fertility clinics. Before ICSI, one egg was placed in a Petri dish with a million or more sperm, in hopes that a single swimmer would penetrate the egg, just as in a middle school sex-ed video. Leaving such a critical part of the IVF process up to chance no longer makes sense, not to doctors and certainly not to the women who have gone through so much to get to this point.
-
 Shawnee Barton.
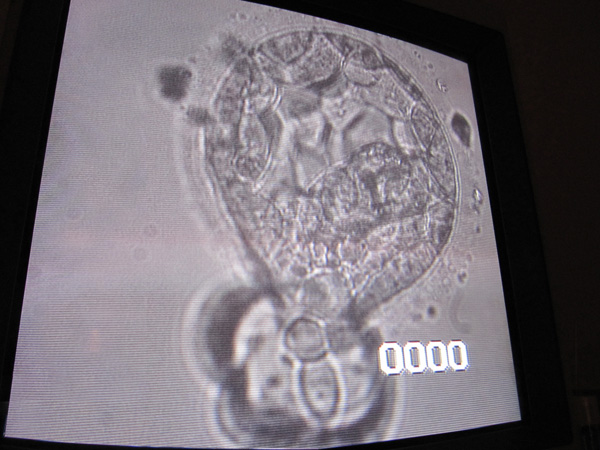
Shawnee Barton.The Beginning of a Life
Even after fertilizing an egg, there is no guarantee an embryo will grow. Several days later, the embryologist looks at her Petri dishes under a microscope to see whether any of the eggs has transformed into a blastocyst—the cluster of five cells that will eventually divide and divide again until it becomes a baby. When she shows us this image of the blastocyst that will eventually be implanted in me, I start to cry. Here is the beginning of a life. And when she tells us that not just one but six of my 11 eggs have matured into embryos, Mike cries too.
-
 Shawnee Barton.
Shawnee Barton.Implantation Day
For implantation, the doctor and team of nurses are back. Once I’m on the exam table, Dr. Agarwal’s partner, Dr. Gabriel Garzo, uses a catheter to snake the blastocyst inside my uterus. Placing the embryo in the exact spot that will give it the best chance of successfully implanting—the best shot at life—takes skill and concentration. Watching him work, I think, “This is why he earns the big bucks.”
Everyone stares in awe at the ultrasound screen as the doctor releases the embryo. It’s the closest thing to a miracle that I have ever seen. Later, a nurse tells me, “That part of my job never gets old.” In many professions, it takes ego to be a star. Before Dr. Garzo leaves the room, he encourages everyone to congratulate me on my pregnancy. I am taken aback by his confidence, but my sense of anticipation is intense. At this moment, I feel so close to the life I want. It will be two excruciatingly long weeks before we know if he is right.
-
 Shawnee Barton.
Shawnee Barton.Babies on Ice?
After Dr. Garzo implanted one embryo, our five remaining blastocycsts were moved into these freezers. Intellectually, I understand that blastocysts aren’t babies at all; they are simply clusters of cells with a lot of potential. Even so, it’s hard not to get sentimental when I think about our “babies on ice.” Besides Mike and my unborn child, they are the most precious things in world to me. All of our biological children will be years apart in age, but their journeys will have started just minutes apart on the same stainless steel lab table.
-
 Shawnee Barton.
Shawnee Barton.Pregnant
Even as I see our baby on the screen at 12 weeks and hear her heartbeat, she seems too good to be true. Family and friends told us to try for a year before worrying. I think now that people say that only because they don’t know what else to say. I wouldn’t walk around with a broken arm without a cast, so it seems silly that I didn’t seek help with our efforts to conceive sooner. Learning to see infertility as a physical problem has left me angry that so few states require insurance to cover any costs related to it.
-
 Shawnee Barton.
Shawnee Barton.Charlie
Last November, our little girl, Charlie Grace Merriman, was born. Just after her birth, I overheard Mike describing her to his mom over the phone. “I wish there was a word for 'more perfect than perfect,' ” he said. I couldn't agree more.
Two thirds of IVF procedures on healthy women under 35, women like me, fail. We easily could have gone through multiple IVF cycles without having a baby. There doesn’t seem to be any rhyme or reason as to why some cycles work and others do not. That first doctor we saw put our odds of conceiving at only 5 percent. That number keeps popping in my head as I look at our beautiful Charlie, and I feel so lucky.