Will Robots Steal Your Job?
Why the highest-paid doctors are the most vulnerable to automation.
The Pap smear is the most effective cancer-screening test ever developed. When it was introduced in the United States in the 1940s, about 26,000 women died every of year of cervical cancer. Today, the exam—now known as the Pap test, since the modern method of preparation no longer requires smearing cells on a slide—is performed about 55 million times a year in this country, and about 120 million times annually worldwide. The effect of widespread, routine testing has been dramatic: Fewer than 5,000 American women now die each year of cervical cancer. If you account for population growth since the 1940s, the Pap test has reduced cervical cancer mortality by more than 90 percent.
The Pap test isn't just good for women. It's also a good business for doctors and diagnostic laboratories—maybe as much as a $500 million industry in the United States. The techs and doctors who look at Pap slides are the TSA agents of the medical world: They spend their days examining dozens of slides in search of tiny, subtle, and rare visual cues of disease. The process begins with a doctor collecting a sample of cells from a woman's cervix. The cells are preserved in liquid, mixed with laboratory reagents, separated from blood and other biological material by centrifuge, and then deposited onto a slide. The cervical cells are examined first by cytotechnologists—specialists trained to analyze certain types of medical slides. If abnormalities are found, the Pap slides are then screened by pathologists, medical doctors who diagnose disease. Because the vast majority of Pap tests are performed on healthy women, about 90 percent of the slides seen by a typical lab are completely normal. The entire process costs about $25 to $100 per test, depending on the lab's efficiency.

Over the last decade, this routine has been infiltrated by robots. In the 1990s, a North Carolina company called TriPath Imaging began developing an automated system to screen Pap slides. The company was later purchased by the medical technology firm BD, whose latest Pap-screening computer, the BD FocalPoint GS Imaging System, is a marvel of medical engineering. The machine's image-searching software rapidly scans slides in search of more than 100 visual signs of abnormal cells. It then ranks the slides according to the likelihood they contain disease, and it identifies 10 areas on each slide for a human to scrutinize. In clinical studies, researchers found that labs that use the BD FocalPoint catch more instances of cancer and pre-cancerous lesions. (In one study, doctors and technicians working without the robot detected 79.2 percent of abnormal slides; with the robot, 85.8 percent of abnormal slides were found).The FocalPoint also increases throughput. Working manually, a cytotechnologist can analyze about 80 to 90 slides a day (regulations set the maximum at 100 per day). Using the FocalPoint, a human examiner can go through 170 slides per day.
The BD FocalPoint represents the vanguard of a medical revolution: computer-aided diagnosis of disease. In addition to Pap tests, computers are now routinely used by radiologists to analyze mammograms, and a range of similar technologies could upend the way pathologists and radiologists screen for many other ailments. So far, machines have proved useful in detecting abnormalities on images of the colon, the chest, and coronary arteries, and they may soon help doctors analyze prostate and breast biopsies.
Should doctors, like pharmacists, be concerned that computers are coming for their jobs? The radiologists and pathologists I spoke to noted that many computer-aided diagnostic technologies are still at the concept stage; it will take years before they're good enough to be integrated into most practices. The makers of both the FocalPoint and the R2 ImageChecker CAD, which is used for analyzing mammograms, stressed that both technologies need human supervision—in practice, humans are always making the final diagnosis with the help of the machines.
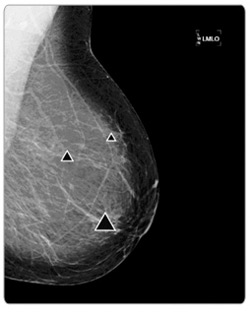
Still, it's certain that doctors' livelihoods will be affected by these new machines. As computers get better, we'll need fewer humans across a range of specialties. Look at mammography: One of the main ways radiologists can improve their breast diagnoses is by "double reading." When two radiologists independently examine a collection of mammograms, the number of cancers detected increases substantially. A study published in 2008, however, found that a radiologist who uses ImageChecker can skip the second reading: A computer and a human are just as good as two humans.
It's not just diagnostic fields of medicine that will feel this pressure. Robotic surgery is on the rise; most large hospitals, and many smaller ones, now have huge, octopus-armed machines that help doctors perform surgeries that are less invasive and more precise. The robots also make surgeons faster, and they allow them to work remotely—a surgeon at a large city hospital can work on patients at satellite hospitals throughout the region. In this way, surgeons could suffer the same fate as pharmacists who will be able to work through telepharmacies—one surgeon could perform the work that currently occupies many.
I've got a personal stake in the rise of medical robots: My wife is a pathologist, and her years of intense training and tough exams have paid off in a nice living for our family. Like the pharmacists I spoke to, my wife and her colleagues acknowledge that computers are making inroads on their work, but they argue that there are too many parts of their jobs that can't be automated. In one sense, they're right; medical tech experts I spoke to say that we won't have fully autonomous medical machines anytime soon. Systems like the BD FocalPoint and R2 ImageChecker will always need human doctors to look over them.
But this doesn't ensure job security for doctors. The economic implications here are obvious. As robots help each doctor do more, there'll be less work for everyone, which will push down salaries. And the doctors who are the juiciest targets for automation might not be the ones you'd expect. They're specialists like my wife—the most highly trained, highly paid people in medicine. It's precisely these factors that make them vulnerable to machines.
By definition, specialists focus on narrow slices of medicine. They spend their days worrying over a single region of the body, and the most specialized doctors will dedicate themselves to just one or two types of procedures. Robots, too, are great specialists. They excel at doing one thing repeatedly, and when they focus, they can achieve near perfection. At some point—and probably faster than we expect—they won't need any human supervision at all.
There's a message here for people far beyond medicine: If you do a single thing—and especially if there's a lot of money in that single thing—you should put a Welcome, Robots! doormat outside your office. They're coming for you.
***
If the most tenuous jobs in medicine are the ones that are the most specialized, then the most secure positions, naturally, are those that require versatility. So, who are the most-versatile doctors? "We like to say that we can take care of 80 percent of the problems of 80 percent of the people," says Sarah Kramer, a family practice doctor in a suburb of Seattle.
Kramer was one of several family practice doctors who answered my survey about how robots are taking over high-skilled jobs, and her story echoed those of other doctors I spoke to. Kramer, who's been practicing for more than 20 years, sees two dozen patients a day. The appointments range widely in length—she can see someone for as few as 10 minutes, and on the rare occasion when she needs to do minor surgery, the session can last an hour. Every patient has a different complaint, too. "If you've got a sinus infection, if you've got a sprained ankle, if you're feeling fine and you need a checkup for work, if you're traveling overseas and you need some vaccines—I'll see you for all of that," Kramer says.
Technology has changed the way she practices medicine. Most of the patients Kramer sees now consult the Web before they come in, and they're usually familiar with basic facts about what's troubling them. But rather than replace Kramer, the Web has deepened her conversations with patients. When she sees someone who's just been diagnosed with high cholesterol, he'll often know he needs to change his diet and exercise plan. "But often I'll have to help them set their expectations," Kramer says. "I'll say, 'I should tell you, that's a good plan—but we have data about outcomes for patients, and from what we know, you'll still be better off if you added some medicine.' "
There are many diagnostic software packages that doctors like Kramer can use to help figure out what's wrong with their patients, and these systems will likely play a larger role in primary care going forward. IBM plans to use the technology in its Jeopardy-winning Watson computer to scour the world's medical textbooks and reference guides for connections between symptoms. A doctor could input symptoms into Watson and get a ranked list of disease possibilities.
But these machines can't replace Kramer's most important skill—the ability to suss out what's wrong with a patient through conversation. These personal conversations wouldn't be easily automated, and unlike consultations between patients and pharmacists, they probably wouldn't work if conducted remotely, either. That's because they depend on Kramer's ability to read a patient's body language, to gauge his emotional state, to determine how sophisticated an explanation he can handle, and to figure out if there are other factors in his life that may affect his treatment. "People are complicated," Kramer says. "You may have a patient who doesn't just have diabetes—he's got diabetes, plus he's just gotten divorced and he wants to start dating again and is worried about sexually transmitted diseases." No robot on the planet could figure out how to treat a patient like this—especially if you consider that patients often lie, mislead, forget to include pertinent facts, and are maddeningly stubborn.
Now, many of these skills aren't confined to primary care doctors. Wherever doctors are talking to patients rather than simply doing procedures on them, you'll find a kind of medicine that's more immune to robotic upheavals. What's ironic, though, is that the doctors who do procedures—people like super-specialized surgeons—who tend to command the highest salaries. The skills that make Kramer a great primary care doctor—the skills that machines can't match—aren't as well remunerated. (Primary care physicians make a median salary of about $163,000, while some surgeons can make four or five times that.)
The pay gap has caused a nationwide shortage of primary care doctors, as many medical students choose the financial rewards of specialization. It's possible that robotics will change this calculus; if machines begin to decrease the need for—and the salaries of—specialists, perhaps primary care will look more attractive. There's some evidence that this would be good for patients and for the health care system. A 2008 study by the American College of Physicians found that when patients visit primary care physicians more often, they receive better preventive care, they require fewer emergency room visits, and patient mortality rates improve. In other words, by turning to robots, we could keep more humans alive.
Of course, this trend would be terrible for specialists like my wife. But as I'll document in my next story, I've got other problems to worry about: Robots are coming for my job, too.