Worked to Death
How victims are shut out of the workers’ comp system by big bills, bad laws, and companies that will do anything but pay.

Photo by Maryam Jameel/Center for Public Integrity
LANCASTER, Pennsylvania—Finding the first bit of evidence that Gene Cooper’s job damaged his brain and destroyed his health was the easy part. That only took his wife four years, eight doctors, and at least a dozen tests.
The hard part: getting his former employer to pay.
Eight years have passed since Sandra Cooper filed a workers’ compensation claim on her husband’s behalf. She prevailed after 4½ years of wrangling, when a judge agreed that chemical exposure on the job at a flooring factory was the reason Gene Cooper—a bright father of two with a quirky sense of humor—had transformed into a nursing-home patient who couldn’t speak and sometimes stared into space when his family visited. That was 2012. Sandra Cooper is still trying to get medical bills and lost wages covered today, nearly two years after he died.
The trouble Cooper has had isn’t unusual for this type of case. What’s unusual is that she’s gotten anything out of workers’ compensation at all.
Americans hurt at work have a difficult enough time with the state-by-state system when their injury is so obvious and immediate—such as an amputation—that it can’t be blamed on anything but the job. When it comes to chemically induced illnesses and other job-triggered diseases that creep up over time, according to researchers and the federal agency overseeing occupational safety, workers’ comp rarely works at all.
“It’s not good, and in many ways, it’s gotten worse,” said John F. Burton Jr., a workers’ compensation expert who chaired a national commission on the subject during the Nixon administration.
The difficulty is partly inherent in the diseases themselves. Most that can be triggered by job exposures—from cancers to lung ailments—have other possible causes, too. Genetics. Smoking. Simple bad luck. Workers have to first suspect their job was to blame and then build a case, gathering exposure information, finding medical experts willing to dig for answers. Most people with occupational diseases never file a claim, researchers say.
But state-run workers’ compensation programs have built additional barriers, often at the urging of industry groups.
In most states, proving that there was a workplace exposure, that it is a known trigger of the illness in question and that, in fact, it was as likely as not the cause of the claimant’s problem, isn’t sufficient. Claimants must show work was more likely to blame than all possible outside causes their employers suggest. In some states, the burden of proof is even higher.
And at least 11 states, including Pennsylvania, Alabama, and Virginia, require most or all sick workers to file claims within several years of their last hazardous exposure, according to a Center for Public Integrity analysis—even though symptoms for a variety of occupational illnesses can take far longer to appear.
The denial rate for disease claims in Ohio and Oregon, rare states that track the outcome of such cases, is three times higher than for injury claims.
The insurance industry points to claimant fraud as a reason for tighter rules, contending that employees and their doctors too often shift costs into workers’ compensation that aren’t due to work. States, employers, and insurers “have to be very careful … in terms of guarding access to the system,” said Robert P. Hartwig, president of the industry-supported Insurance Information Institute.
But J. Paul Leigh, a professor of health economics at the University of California–Davis, found major costing-shifting in the other direction. A study he co-wrote in 2004, partially funded with a federal grant and cited in a 2015 report by the Occupational Safety and Health Administration about how the system fails workers, estimated that more than 95 percent of ultimately fatal occupational diseases are never covered by workers’ comp.
“It was remarkable—unfortunate, actually—the huge disparity between what workers’ compensation paid for and what epidemiological estimates consider are the true deaths attributed to occupational exposure,” Leigh said.
Taxpayers picked up nearly $27 billion in expenses from work injuries and illnesses in 2007 alone through federal programs such as Medicare, Leigh and a co-author estimated in a separate 2012 study. The biggest share of the burden fell on the workers and their families: an estimated $125 billion, or half the cost.
“What’s the Matter With Dad?”
Gene Cooper was 48 the day he struggled home from the flooring plant where he worked in Lancaster, Pennsylvania, coughing and coughing. He told his wife he’d had to help clean up a spill.
That was September 2003. The cough was so persistent that Sandra Cooper made him see a doctor, but soon she had other things to worry about. Her husband—a talented investor who was more than halfway done with a master’s in financial planning—was suddenly having trouble with simple tasks.
“By late October into November, he was mixing up gender, losing proper nouns when he spoke,” Sandra said. “The kids noticed and kept asking, ‘What’s the matter with Dad? What’s going on?’ Really, by Christmas, he was very confused, going to work [at] the wrong time, getting dates mixed up.”
“I don’t know what’s the matter,” he told her right after Christmas of that year, teary eyed.
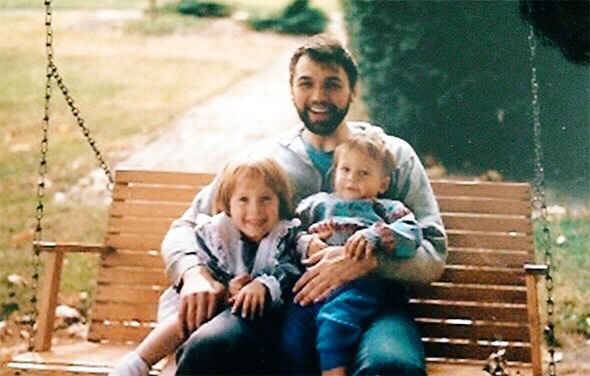
Courtesy of Sandra Cooper
Seven months after the spill, he could no longer work. By 2006, he was in a nursing home, not speaking, his family unable to tell whether he recognized them or not. As his body deteriorated and Parkinson’s symptoms set in, he lost the ability to swallow, and that was how he died in 2014—choking on the aspirated contents of his stomach. It’s an image his wife cannot get out of her head.
The bills to care for him were so massive—hundreds of thousands of dollars’ worth—that they gobbled up his retirement fund, his investments, and his Social Security disability payments. Sandra had to tap their son’s college fund, the inheritance her late mother left her, and lines of credit to keep going.
Her initial efforts to find out whether work could be the cause of his illness went nowhere. The occupational medicine specialist who saw him in 2005 couldn’t help because Sandra had no idea what substances were in the spill. Her lawyer did request her husband’s medical and exposure records that year from his employer, Lancaster-based Armstrong World Industries, and came away empty-handed. Armstrong spokeswoman Jennifer Johnson said in an email that the company needed a request in writing and did not get one. Sandra said the company refused to turn over records at all unless she filed a workers’ compensation claim.
Later, OSHA would cite Armstrong for failing to share exposure information when requested in 2015—a citation the company called minor and said has been resolved. Lawsuits would be filed, alleging that the company intentionally tossed workers’ records into a dumpster, a claim the company denies. The coroner, after Gene’s autopsy, would rule that complications from chemical exposure at work caused his death.
But that was all in the future. At the time, Sandra had nothing to go on to file a claim. Specialists were still struggling to accurately diagnose her husband’s condition, let alone what triggered it. All that was clear was he had some form of dementia.
Then, a doctor filling out paperwork in late 2007 checked a box indicating that Gene’s medical problems were caused by work. Sandra took her first step into the world of workers’ compensation, thinking she would finally get some help.
The system is supposed to be faster, cheaper, and less adversarial than a lawsuit. That’s frequently not how it plays out in state systems across the country, especially for illnesses. Nor was that the case for the Coopers.
Armstrong filed for Chapter 11 bankruptcy protection in 2000 after a wave of asbestos lawsuits—it once installed asbestos insulation—but has been out of the bankruptcy courts for nine years now. The publicly traded company, which reported nearly $240 million in operating income last year, contested the Coopers’ claim as vigorously as a civil-suit defense.
The company first contended the request for workers’ compensation came after the statute of limitations had expired. When that didn’t quash the claim, Armstrong put more than a dozen witnesses on the stand to make the case that Gene had not helped clean up the spill, would rarely have come into contact with chemicals at work, and was suffering not from solvent-triggered brain damage but simply a nonoccupational instance of early-onset Alzheimer’s disease, according to the workers’ compensation judge’s summary of the case.
Sandra had to bring her own medical experts in to testify, racking up tens of thousands of dollars in further costs. The four specialists—two neurologists, a neuropsychologist, and a toxicologist—linked her husband’s dementia and Parkinson’s symptoms to solvent exposure, in part by using brain scans to identify the type of damage. Other witnesses spoke about conditions at the plant, including an Armstrong worker who testified that he saw Gene coming up from the basement where the spill cleanup was in progress.
The judge, detailing all this in a 96-page decision letter, declared the claim compensable. Gene had indeed been exposed to hazardous chemicals as a result of the spill—which occurred while the area was left unattended so workers could go to a safety fair—and over the course of a three-decade career with Armstrong, mostly as an inspector, wrote Judge Tina Maria Rago. Those chemicals included a carcinogenic and neurotoxic solvent called trichloroethylene. Armstrong “admitted the existence of these chemicals” in the plant after the Coopers’ witnesses testified to it, Rago wrote.
But that 2012 decision was far from the end of it. Though largely upheld by the Pennsylvania workers’ compensation appeal board, the original decision was narrowed by the board’s 2014 finding that the company would not have to pay compensation to Sandra for the three and a half years between her husband’s last day of work and the date she was finally able to file the claim. Until notice was provided, “no compensation was due,” the board ruled.
Meanwhile, a forensic accountant she hired to sift through her records testified in July that $364,000 in out-of-pocket medical expenses for Gene—from before and after the contested 3½-year period—remained unreimbursed. Large amounts of interest and post-claim lost wages also have not been paid, the accountant testified. Sandra said it was only in August, years after the decision, that she received any reimbursement for medical costs incurred after the claim was filed.
Armstrong’s Johnson wrote in an email that the company, while unable to speak in detail about a pending case, has “fully complied with the workers’ compensation decision addressing Mr. Cooper’s medical bills.” She did not address the issue of wages but said some of the medical expenses are “under review or in dispute.”
“We recognize and respect that an employee who is hurt or harmed in the workplace is entitled to pursue a worker’s compensation claim. However, if the claim is erroneous or unfounded, the employer has the right, and arguably the duty, to contest the claim, which is exactly what we are doing,” Johnson wrote. “For example, with respect to Mr. Cooper we do not believe the medical conditions outlined in his case were caused by chemical exposure in the Armstrong workplace. That matter … is currently under appeal by both parties.”
Safety, including proper handling of chemicals, “informs everything we do and is our number one priority,” Johnson added.
Word of Sandra Cooper’s battle with Armstrong slowly spread. One by one, people approached her—other sick former workers from that flooring plant. Some of them had Parkinson’s, like her husband. Others had cancer, particularly multiple myeloma, a rare bone-marrow condition some studies link to solvent exposure. Sometimes it wasn’t the workers themselves but their survivors who came to her.
None had filed a workers’ compensation claim for those illnesses. A few had only suspected a work connection; for most, the possibility had never crossed their minds. Now it was too late to file a claim: Pennsylvania’s deadline, set in 1972, is a few months shy of six years after the last on-the-job toxic exposure.
Appellate court opinions suggested the purpose of the cutoff was to “prevent stale claims” and “prevent speculation over whether a disease is work-related years after the exposure occurred,” according to the Pennsylvania Department of Labor and Industry.

Photo by Maryam Jameel/Center for Public Integrity
The former Armstrong workers and their families came to Cooper with the same question: What should they do?
“Grand Bargain”
Workers’ compensation developed a century ago in the country, state by state, as an attempt to fix a broken system. Injured employees rarely prevailed in court, because laws at the time immunized companies from liability if the worker contributed to his injury in any way—even by slipping. Employers, meanwhile, had to defend themselves frequently enough—occasionally with big-ticket losses—that they were anxious about costs.
Workers’ compensation was pitched as a “grand bargain”: Injured employees would get medical and wage assistance without having to prove negligence while employers would not have to pay for pain, suffering, or punitive damages.
This new system wasn’t merely an alternative to lawsuits. It was—and remains—a substitute. With rare exceptions, typically in cases involving a clear intent to harm, the only option for people seeking compensation from their employers for on-the-job injuries or illnesses is workers’ comp.
When workers’ compensation systems were first set up in the United States, the major known risk an employee faced was traumatic injury. Mine explosions. Train derailments. Machinery malfunctions. Hazards were ever-present: Some 23,000 people died in U.S. industrial accidents in 1913.
Now, though, deaths from occupational diseases outnumber fatal work injuries 9 to 1, according to a 2011 analysis by Leigh, of the University of California–Davis. But workers’ compensation still handles injuries better than illnesses, said Burton, the workers’ comp expert and a professor emeritus at both Rutgers and Cornell universities.
The denial rate is markedly higher for disease claims than for injury claims in the few states that track that statistic. In Oregon, for example, 36 percent of disabling-disease claims were denied in 2014, compared with 11 percent of disabling injury claims. In Ohio, disease claims were denied nearly half the time in 2014, compared with just 14 percent of injury claims.
When workers’ comp does pay for an occupational disease, it’s far more likely to be a condition such as tendinitis or carpal tunnel syndrome than potentially deadly illnesses such as cancer, Leigh found in 2004.
Rules written decades ago and never changed are part of the problem. At least 11 states, for instance, set the worker’s deadline to file a claim for most or all diseases based on the time elapsed since the last exposure to the hazard—not when the person was actually diagnosed with the illness. In those states, the window generally closes in one to seven years.
Silicosis, a lung disease triggered by the silica dust that can shroud a badly run construction site, typically takes 10 years or more to develop. Bladder cancer, which can be set in motion by coal tar, metalworking fluids, and other workplace toxics, usually appears 15 to 40 years later. Mesothelioma, a cancer caused by asbestos, almost always lies latent for decades. Other such examples abound.

Photo by Maryam Jameel/Center for Public Integrity
The National Commission on State Workmen’s Compensation Laws said in 1972—43 years ago—that deadlines should be set after employees become aware that they have an occupational disease, given the “substantial lag” that can come between exposure and diagnosis. At that point, about half the states didn’t meet that test.
Iowa is one of the states that still don’t. If workers there do not become disabled or die within one year of the last “injurious” exposure, or three years if the hazard causes one of the lung diseases categorized as pneumoconiosis, they have no recourse. The only exception is for diseases involving radiation, in which case workers are allowed to actually find out that they have a disabling occupational illness before the clock starts ticking.
Paul J. McAndrew Jr., an Iowa lawyer who has represented employees in workers’ compensation cases for 25 years, called the state’s deadline rule “a patent injustice” that requires him to tell very sick people that they have no legal remedy against their former employer. Usually, the people he is able to help file a claim are those still employed at the site that made them ill.
He was part of a brief effort just over a decade ago, when Iowa made changes to workers’ comp, to get the deadline altered. Workers’ advocates proposed to start the clock ticking when the disease is discovered. That idea was immediately batted down, McAndrew said.
“When we negotiated in 2004, the only message coming back from defense side that made any sense at all was, ‘This one is too valuable. We won’t even consider it,’ ” he said. “It’s a well-known cost savings to the insurance industry. That’s what it is.”
Other barriers are part of a more modern effort by states to lower workers’ compensation costs for employers.
“Over the past 25 years, states have made it much harder for both illnesses and injuries to receive workers’ comp benefits,” said Les Boden, an economist and a professor of environmental health at Boston University.
Mississippi and Louisiana, for instance, both rewrote their laws in 2012 in an effort to overturn court precedent that rules be interpreted in favor of workers when resolving disputes. Many states have raised the level of proof a worker must meet from essentially 50-50 to a higher standard, usually a preponderance of the evidence, according to Emily A. Spieler, a law professor at Northeastern University who once headed the West Virginia workers’ compensation system.
With the waning of union power, there’s been little organized effort to push back, Spieler said.
Preponderance of the evidence is a typical civil-suit standard. Charles Davoli, a Louisiana lawyer who is past president of the Workers’ Injury Law and Advocacy Group, argues that the original intent of workers’ compensation was to make it easier than suing—since employees gave up their right to the higher payouts civil cases can bring. Changing that, he said, “is all about cost mitigation.”
Lawyers who represent companies or insurers see a 50-50 standard as too low for a properly functioning system.
“Because these things are very easy to allege and very difficult to investigate and disprove, I think at least from my perspective, it’s not unfair to have a heighted burden of proof,” said Bill Scherle, a workers’ compensation lawyer in Iowa who largely focuses on defense work.
Some states apply a still-higher standard of clear and convincing evidence, either for all occupational diseases or if the claimant’s condition can be classified as an “ordinary disease of life”—conditions the general public could contract, even though certain jobs can increase the risk of developing them.
Virginia has that type of rule. And with the exception of hearing loss and carpal tunnel syndrome, the state doesn’t define whether a condition is occupational or ordinary, leaving the parties to argue it out in front of the program’s judges, according to the Virginia Workers’ Compensation Commission.
Douglas Landau, a workers’ compensation lawyer in Virginia, had to prove a client who baked rolls at a middle school—and developed a nondisabling lung ailment after daily exposure to flour dust—had no outside exposure of even a minor nature. He put a witness on the stand to testify that his client did not, in fact, bake the cakes she brought to monthly Elks Lodge meetings.
Landau takes workers’ compensation cases in other states as well but said a lot of clients, once they learn about the difficulties, opt to seek disability help from Social Security instead. The burden of proof makes it “extraordinary difficult” to win an occupational disease claim in workers’ compensation, he said, “even if you’ve only had one employer your entire career and even if the offending toxin or particle can be identified.”
Trey Gillespie, senior workers’ compensation director at the Property Casualty Insurers Association of America, a trade group, agrees that workers face difficulties with proof. He sees lack of medical evidence as the major problem, not the system itself. If you develop cancer and ask your doctor what caused it “quite often, the doctor will say, ‘I don’t know—it could be lots of things,’ ” he said.
“I think the workers’ comp system is prepared to take care of workers that have an illness that scientific research supports … is occupational in nature, but until the scientific research hits that level, then basically the burden really falls upon other private-payer systems or the public-payer system to help employees that have that illness,” Gillespie said.
Some of the people shut out of workers’ compensation by deadlines, rather than medical evidence, have turned to the courts for help—with varying results.
Iowa’s highest court ruled in 1991 that employees cannot collect workers’ compensation for diseases discovered after that state’s deadline and then ruled in 1998 that such workers also could not sue their employers.
But Pennsylvania’s highest court, considering two cases brought by mesothelioma victims, went the other way in 2013.
“It is inconceivable that the legislature, in enacting a statute specifically designed to benefit employees, intended to leave a certain class of employees who have suffered the most serious of work-related injuries without any redress under the Act or at common law,” the majority of the justices wrote.
In Pennsylvania, if the disease manifests after the workers’ compensation deadline of 300 weeks from the last exposure, an ill worker has no remedy in that system. Therefore, the justices ruled, he or she can sue.
Since July, about a dozen former Armstrong workers—or their survivors—have done just that.
The Plaintiffs

Photo by Maryam Jameel/Center for Public Integrity
Don Roberts worked at the Lancaster plant for 27 years, until downsizing hit in 1997, and was employed at a medical-supplies firm when he began to have balance and memory problems. It was Parkinson’s, a diagnosis that came as a shock seven years ago.
Now 64, Roberts had to take his Armstrong pension early—slicing his payments in half—so he and his wife wouldn’t lose their house. Covering his health insurance cost them about $700 a month for the 3½ years before he qualified for Medicare. And in August, to improve his symptoms, he underwent brain surgery that required him to remain conscious while two holes were drilled into his skull.
“It’s just a Band-Aid,” said his wife, Marilyn Roberts. “There’s not a cure for this, not at this point.”
The Robertses are among those suing Armstrong, all of whom are represented by Sandra Cooper’s lawyer, George Chada, a toxicologist-turned-attorney. The lawsuits contend that Armstrong triggered diseases by regularly exposing workers to a product called Safety Solvent. A 1989 Armstrong purchase document and a 2008 fax—turned up as part of Cooper’s fight against the company—both give the product’s components: largely methylene chloride and trichloroethylene with some methyl ethyl ketone thrown in for good measure.
Trichloroethylene is a known human carcinogen; methylene chloride is considered a likely cancer-causing agent. Trichloroethylene in particular is associated with a variety of ailments—Parkinson’s, liver and other cancers, neurological problems, and kidney damage among them. It’s one of the chemicals implicated in illnesses and deaths among people who worked and lived at the contaminated Camp Lejeune Marine Corps base in North Carolina.
The former Armstrong employees worked in their street clothes, which they wore home to be laundered, and they now worry about the implications for their families. The Robertses’ son, Jason, was born with only one kidney and is a co-plaintiff in their lawsuit.
Johnson, the Armstrong spokeswoman, wrote in her email that the company has not seen any evidence supporting “that any of the medical conditions identified in the plaintiffs’ complaints are as a result of their employment at Armstrong.” The company does not use the solvent described in the pending lawsuits, she wrote, “and if we ever used the particular type of solvent to which you refer, it would have been many years ago.”
“In all of our plants, we follow and often exceed all applicable safety requirements, including those relating to protocols for working with chemicals and the use of proper protective equipment,” Johnson wrote.
The lawsuits also contend that Armstrong purposely destroyed medical and exposure records. One exhibit includes an affidavit from an employee who attests to witnessing this last year and a string of photos showing boxes and file folders tossed in a dumpster. (Cooper filed a lawsuit against Armstrong, too; it focuses on such concealment-of-information allegations.)
OSHA, looking into the dumping allegation because companies are required to share such records with employees when asked, couldn’t conclusively prove what was thrown away. Johnson said the binders and boxes were empty. But OSHA cited Armstrong in September for failing to give medical and exposure records to a former employee’s representative when requested.
Johnson said the OSHA citation involved “a few non-substantive administrative items” and has been resolved. She said the company has turned over tens of thousands of pages of medical and exposure records to the plaintiffs’ lawyer.
Several of the lawsuits involve cases of multiple myeloma, linked in some studies to trichloroethylene and methylene chloride. Judy Wendler’s husband, George, who worked at the Lancaster plant for 30 years, died of the condition last year at 65 after a nearly six-year struggle.
Wendler, a registered nurse, had to keep working while caring for him in order to stay insured—she’s still not sure how she managed. Despite the insurance, and Medicare eventually kicking in, she amassed thousands of dollars in credit-card debt to cover his health care expenses.
“It just really took a toll on the whole family,” Wendler said. “His bones became brittle from the multiple myeloma; they more or less were eaten away, is what we were told. … But he made himself do things, in great pain.”

Courtesy of Sherry Riley
Sherry Riley is another plaintiff. Her husband, Jeffrey, who worked at the Armstrong plant from 1986 to 2000, was just 47 when he died five years ago from leukemia. His loss was a devastating emotional and financial hit she is still trying to recover from. She had to borrow money recently to keep her house out of tax sale.
“I’m getting my electric shut off, I’m on food stamps, I’m selling things … I’m trying everything I can,” Riley, 54, said this summer.
Then there’s Michael Moeller, who worked at the Lancaster plant for more than two decades before transferring to other Armstrong facilities. His 2010 death at age 50 was so mysterious that it took the coroner’s office almost 3½ years to determine the cause: acute severe hemolysis triggered by trichloroethylene exposure. The chemical set off an autoimmune reaction in which his body attacked his own red blood cells.
“He essentially suffocated to death,” said Stephanie Bernstein, his sister.
At his parents’ house in Lancaster, a photo collage his family made for his funeral shows him as a baby, a child, an adult, always with the same sunny smile.
“It was the worst shock when that coroner called,” his mother, Marie Moeller, 77, said in October.
A few months earlier, just up the street, former workers and spouses filled up the seats in Sandra Cooper’s living room. They talked about conditions in the 106-year-old plant, particularly in the ’80s and ’90s. The stench of chemicals, they said, was ever-present.
Marilyn Roberts turned to her husband and asked, “Don, did you ever have any protection at all?”
“We had gloves on,” he said, pressing one of his hands to the other to try to control the tremors. “That’s all we basically had.”
What’s the Fix?
In 1972, President Richard Nixon’s National Commission on State Workmen’s Compensation Laws declared that the states’ programs were, “in general, inadequate and inequitable.” Burton, who chaired that commission, said the states did better for a while—trying to stave off the possibility of federal intervention—but have backslid since.
He doesn’t hold out much hope of reforms to help ill workers in the current environment.
“Politics in many states are pretty conservative,” he said. “I think the problem you’ve got right now is the problem the national commission wrestled with, which is, left to their own devices the states are in a race to the bottom.”
The Insurance Information Institute defends the current workers’ compensation setup. The rules in place, the group says, are necessary.
“Unfortunately, there’s a long history of fraudulent behavior and efforts to shift costs into the workers’ compensation system,” said Hartwig, the group’s president. “In order to keep workers’ comp costs manageable for everyone, it’s important that the system have a very prescribed manner in which eligibility is determined and compensation is made.”
The institute pointed to statistics from the National Insurance Crime Bureau, a nonprofit that helps fight insurance fraud. Insurers referred about 3,500 questionable claims involving workers’ compensation to the NICB in 2011 and about 4,500 in 2012, according to the group’s most recently released figures.
But both figures amounted to about 0.1 percent of total workers’ compensation claims and include potential fraud by companies—such as undercounting employees to reduce premiums—as well as workers or doctors.
Texas Mutual Insurance Co., which has 40 percent of the workers’ compensation market in that state and aggressively investigates fraud, found $5.3 million in employer fraud last year, six times the amount of claimant fraud it discovered.
Some health advocates see a nationally run system—or at least active oversight from the federal government—as part of the solution to workers’ compensation woes. Indeed, after taking responsibility for administering benefits to coal miners for black lung, the federal government did once contemplate handling other occupational disease claims.
In 1980, the Department of Labor issued an interim report suggesting such a move as one of several options to improve a situation in which, the agency noted, people with job-related illnesses rarely received help from workers’ compensation. Social Security and welfare programs were left to pick up costs amounting to $2.2 billion annually, the agency said.
Glenn Shor was one of the analysts working on that report in the agency’s Office of Health and Disability. Nothing ever came of it, he said. After Ronald Reagan was elected, Shor said, the study group was disbanded.
But the interim report outlined ways to make the challenge represented by occupational disease somewhat less daunting, whether in a state or federal system, including better data collection and presumption standards to reduce the difficulty workers have proving the cause of their disease. The report also discussed how to ensure that companies rather than taxpayers footed the bill—for instance, by levying a tax on disease-prone industries.
That’s important not only to make sure ill workers get treatment, said Shor, a member of the occupational health and safety section of the American Public Health Association. It’s about incentivizing companies to reduce health hazards so the illnesses don’t happen in the first place.
“If you don’t have to pay for it,” Shor said, “you’re not going to do much to prevent it.”
A Workers’ Comp Case Drags On
Sandra Cooper sat quietly as her lawyer’s voice filled a small Lancaster hearing room in July. George Chada did not hide his frustration.
Robert J. Goduto, the workers’ compensation judge who took over the case after the 2012 decision finding it compensable, had not allowed one of Cooper’s financial experts to testify. When Chada asked that Armstrong be made to disclose more information about its payments related to the claim, the judge’s response was to calmly ask him to sit down. And now, Armstrong’s lawyer was arguing that the appeals board decision from the previous November—the one that said the company would not have to pay “compensation” for the 3½ years before the claim was filed—should extend not only to lost wages but also to medical expenses.
Goduto expressed interest in the case law on that point, but he did not entertain Chada’s request to present evidence that the company did not turn over information that could have helped Cooper file the claim years earlier.
Chada jumped up again, outraged: “So you’re going to allow the employer to conceal its notice, and then get a credit for concealing its notice? That would reward a fraud!”
“Please have a seat,” Goduto said.
Two months later, three workers’ compensation judges—Goduto among them—gave a seminar for the Lancaster Chamber of Commerce and Industry. The talk was billed as an opportunity to hear the judges “discuss pointers on how employers can be successful in workers’ compensation litigation.”
Cooper couldn’t believe it when she saw an announcement for the event. Armstrong is a member of the chamber. She filed a pending motion citing this and asking for the case to be reassigned back to the original judge.
Goduto, who represented companies in workers’ compensation matters before becoming a judge, declined to comment. Sara Goulet, a spokeswoman for the state Department of Labor and Industry, said by email that she could not speak about specific complaints but added that judges’ discussion at such seminars focuses on the process, “not how to win a case.”
Cooper can appeal the issue of the unpaid 3½ years to Pennsylvania’s Commonwealth Court. But she has to exhaust all her appeals within workers’ comp first. She thinks her case shows how, even when a claim is approved, the system benefits employers and insurers because delays primarily harm cash-strapped claimants.
“The longer they drag it out, the longer it takes to get paid,” she wrote in an email, “and the more legal costs I incur.”
It has eaten up her life, this conflict, and forever altered it. She was a high school art teacher, and now she navigates the complex world of chemical exposures and disease causation, helping others just starting down the same road.
Sitting in her living room this summer, she recalled how her husband—back when they were in their 30s or early 40s—would turn to the obituary section of the local newspaper and exclaim that some guy or other he’d worked with had died. Usually the man had just retired, she said.
Only later did the possible connection to work hit her. She’s sobered by the thought that this is a national problem, not just a Lancaster one.
“People, they don’t connect the dots. I mean, people do get cancer. If you don’t know anything about toxicology, and who does, how would you possibly know that [work could be the cause]? You just don’t,” Cooper said. Workers in that situation can’t hold companies to account, she added, “and that’s what they bet on—that people don’t know.”
This story was published by the Center for Public Integrity, a nonprofit, nonpartisan investigative news organization in Washington, D.C.