The American Way of Dentistry
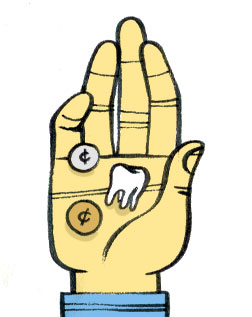
Why poor folks are short on teeth.
So far, I've focused on the 152 million Americans with dental benefits. That ignores the 21 million enrolled in public programs (mostly Medicaid) and the 130 million—43 percent of the population—without any kind of coverage. American dentists provide outstanding care to the people who can afford it, but they are failing the other half of the nation that can't.
The main problem is a lack of decent low-cost options. Chester Douglass, emeritus professor in the department of Oral Health Policy and Epidemiology at Harvard's School of Dental Medicine, puts it this way: "If you want to buy a good, inexpensive car, Volkswagen proved you could do it, then other people started being able to do it." The Volkswagen of dentistry has yet to be built.
In 2007, the difficulty Medicaid recipients experience acquiring dental treatment hit the news when Deamonte Driver, a 12-year-old from Prince George's County, Md., died after bacteria from an untreated dental abscess spread to his brain. His mother, Alyce Driver, had tried with little success to get dental care for Deamonte and his younger brother, DeShawn, who also suffered abscesses related to rotting teeth. Driver was able to enlist the help of Laurie Norris, a lawyer who worked with homeless families, but a Washington Post story reported that Norris and her staff had to make more than two dozen calls before they could locate a dentist who would treat Driver's boys. Driver arranged a cleaning, an X-ray, and a referral for consultation with an oral surgeon for DeShawn, but before Deamonte could be treated, Driver lost her Medicaid coverage (possibly as a result of official paperwork going astray, a constant problem for families without a fixed address).
The Deamonte Driver case was unusually tragic in its particulars, but it served to inform the larger public that only about 900 of Maryland's 5,500 dentists were accepting Medicaid patients and that fewer than one-third of all children enrolled in Maryland's Medicaid program were receiving dental care. (The proportion for Virginia was even lower.)
If you have no money and your appendix bursts, you can walk into a hospital emergency room. If you have no money and your teeth hurt like a son of a bitch, you can walk into a hospital emergency room, but it won't do you much good. According to a 2003 study published in the Annals of Emergency Medicine, an average of 738,000 people visit an emergency department for tooth pain or injury each year. In Washington's King County, which includes the city of Seattle, dental issues represent three of the top 10 factors driving uninsured patients to the ER. The problem is, most hospital emergency rooms have no real way to treat dental problems. They can provide pain medicine and perhaps an antibiotic for the infection—but after that, they can do little more than offer a list of dentists who might be willing to treat the diseased teeth.
Dentists often cite low fees to explain their reluctance to see Medicaid patients. "You can't drive a delivery-care system on charity," a representative of the Washington State Dental Association told me. On average, around 60 percent of dentists' fees are eaten up by the costs of doing business. Medicaid reimbursement levels vary by state, but in Washington state, they're little more than half of usual and customary rates, and dentists claim they don't cover their costs. Another frequent complaint concerns Medicaid's onerous paperwork and slow payment. "The time lags for getting paid by the state are three to six months," says WSDA's Bracken Killpack. "You can't take that hit on your receivables."
Others argue that this is not the whole picture. Columbia's Burton Edelstein points to unpublished research conducted by one of his Columbia graduate students that stated, "in a substantial portion of the states, the package of common pediatric dental services exceeds 60 percent of dentists' usual and customary charges." When states have raised Medicaid fees, the result has typically been an increase not in dentists' participation rates but rather in the number of patients treated by dentists who were already participating. Edelstein also says Medicaid's paperwork demands are no more daunting than those imposed by private health insurers.
Edelstein, who worked for many years as a pediatric dentist in a Connecticut practice where one-third of the clientele were Medicaid patients, observes that there are many cultural "disconnects" separating Medicaid beneficiaries and dentists. "Geographic disconnect, social disconnect, language disconnect, dentist treatment comfort disconnect—we're talking about young children with extensive dental disease, and these are often not the patients that dentists prioritize in their practices." In Edelstein's view, the most effective way for a dentist to treat a low-income population is to relocate to a lower-income neighborhood or along bus routes heavily trafficked by the poor and to "staff more with people who look like and can relate to the population you're targeting—which is what we do now on the affluent end."
The geographic mismatch is especially severe for the rural poor. In 2000, there were 224 counties in the United States without a single dentist and many more with just one or two. Given the expenses associated with a solo dental practice, it makes little economic sense to set up shop in a place where few people can afford your services. In Seattle, I heard about a pattern that has been repeated all over the country: As it became more expensive to live in the city, low-income families drifted farther out, particularly to South King County. There were very few dentists already practicing in the area, and since it costs so much to set up a new office or community health clinic, the new residents cannot get care. Even a relativelyaffluent rural population may be too small to support a dental practice, given that most people go to the dentist only once or twice a year, and then usually just for a cleaning.
Deamonte Driver's story showed that letting one part of the body literally rot can create havoc in other parts. New York University College of Dentistry Dean Charles Bertolami has noted that dental bacteria have been linked in studies to "cardiovascular disease, diabetes, pneumonia, and pre-term, low-birth-weight deliveries." In Uninsured in America: Life and Death in the Land of Opportunity, Susan Starr Sered and Rushika Fernandopulle write:
Dental problems frequently mix and match with other chronic disease to create illness cycles that prove especially difficult to break. Because they affect the ability to chew, untreated dental problems tend to exacerbate conditions such as diabetes or heart disease. Being limited to soft foods is particularly problematic for people with diabetes, who must be careful to eat well in order to control blood sugar levels. Missing and rotten teeth make it painful if not impossible to chew fruits, whole-grain foods, salads, or many of the fiber-rich foods recommended by doctors and nutrition experts. Typical daily diets for those who cannot chew tend to include large quantities of processed lunch meats, canned potatoes, and cream soups—food choices that are particularly bad for people with diabetes. To make matters worse, healthy foods also tend to be more expensive.
There are also intangible but no less powerful reasons to maintain dental health. When I asked Harvard's Chester Douglass why keeping natural teeth mattered, he told me: "If you enjoy chewing; if you enjoy speaking; if you enjoy social interaction; if you enjoy having a job—a responsible position—you've got to have oral health. So the question becomes how important is eating, speaking, social life, and a job?"
In a country in denial about class divisions, a mangled mouth is the clearest indication of second-class citizenship. Missing or rotting teeth are like a scarlet T, declaring their owner to be trash. Sered and Fernandopulle describe the way that a group of well-meaning Idaho women who volunteered at clinics and early childhood development programs judged "those people" who weren't able to get dental care for themselves or for their children. "These middle-class women," they wrote, "identified bad teeth as a sign of poor parenting, low educational achievement, and slow or faulty intellectual development." When Stu Price, Ed Helms' character in The Hangover, wakes up in Las Vegas and discovers he is missing a front tooth, his horrified response is to declare, "I look like a nerd hillbilly." Every lazy screenwriter knows how to label a character as a menacing half-wit: give him gnarly teeth and a sleeveless T-shirt.
Next: Inside the Dental Safety Net
Click here to see a video slide show about the painful history of dentists in the movies. Got a dentist story to tell? Become a fan of "The American Way of Dentistry" on Facebook.
