Here’s an honest question: What is the point of knowing that a gene called KRAS is mutated in many colorectal cancers? Or knowing that p53 is mutated in several types of cancer? Or knowing any of the hundreds of genetic mutations that appear in tumor cells across the land? Unless you work in an academic or industry laboratory, what is the use of knowing the genetic mutation responsible for a cancer? For almost every known cancer mutation, there is no drug to match it with.
The understanding that genetic mutations are linked to cancer is decades-old; the first human oncogenes (genes that trigger cancer) were found in the early 1980s. The exponential growth of cancer genomics is the legacy of the Human Genome Project and spin-off projects like the Cancer Genome Atlas, a publicly funded, collaborative project to parse the genetic underpinnings of cancer, as well as technological advances that allow rapid extraction of genetic information. A single DNA sequencer can now accomplish in a day what took 10 years for the Human Genome Project—and for thousands of dollars per genome, versus $100 million in the olden days of the 1990s. The deluge in genetic information will continue for some time.
The most famous abnormalities are variations of the BRCA gene known as BRCA1 and BRCA2, which can gravely increase the risk of breast and ovarian cancer. These mutations are usually inherited. But cancer genomics has uncovered hundreds of genetic mutations that arise spontaneously during a lifetime. These abnormalities can’t be predicted or prevented—or, on the plus side, passed on to one’s children. There’s SF3B1 in myelodysplastic syndrome, a type of blood cancer. Abnormalities in a gene called FLT3 (pronounced flit-3) are common among patients with acute myeloid leukemia. Many brain tumors have abnormal IDH1 genes. Mutated versions of MLL2 and MLL3 have been found in medulloblastoma, non-Hodgkin lymphoma, prostate cancer, and breast cancer (PDF). And on and on.
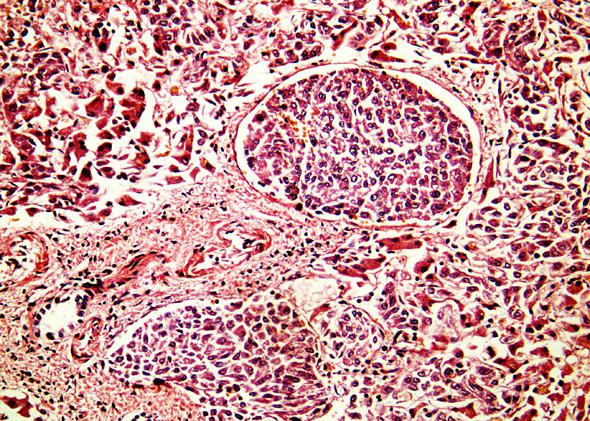
Science has come far in deciphering not only what genes are mutated in what cancers, but also how and when the changes arise. The knowledge is remarkably specific. According to recent research, the most common solid tumors (that is, cancer that occurs as clusters of cells in or on organs, rather than in liquid form within the blood or lymphatic system) have up to 66 mutations that influence how the cancer cells operate—how fast they divide, whether they are susceptible to the signals that would normally cause a cell to die, when they detach from the main tumor to colonize another organ in the body, when and where they attach blood vessels to healthy tissues. Most of the functions that allow cancer cells to flourish are made possible by genetic mutations.
All told, about 140 genes have been found that, when mutated, can drive the development and progress of cancer. These are the “driver mutations,” which are often accompanied by “passenger mutations,” abnormalities that occur as cancer progresses but do not spur the disease. Most tumors contain fewer than 10 of the driver mutations, but the number of total mutations—passenger and driver—can climb far higher, from a dozen or so in neuroblastoma to approximately 200 in lung cancer.
The reason cancer-causing mutations occur follows a cold logic. Simply, it’s largely a matter of odds. When a cell divides, its DNA double helix unzips so that the genome can be copied, one for each of the daughter cells. (Here’s an explanation in rap.) Our genetic information is encoded by the nucleotides thymine, cytosine, guanine, and adenosine, abbreviated as T, C, G, and A, respectively. Each of our 20,000 or so genes is made up of a sequence of those bases. Strung together and squished into chromosomes, our genome contains a total of 3 billion bases. The Human Genome Project produced reams of data that look like this: TCGGGAAATTCGATCCCCAAAATTCTA, etc. (You can see genetic sequences online here.)
That’s the miracle of life, or one of them. Every single cell in our bodies contains a complete copy of the human genome. If you unwound the DNA from all these cells, it would reach to the sun and back 400 times. And every time a new cell is made, which is often—about 10 trillion times in a lifetime—the genome is copied, from the moment of conception to the moment we shuffle off this mortal helix.
That’s a lot of T’s, C’s, G’s, and A’s, and sometimes mistakes happen during replication. Sometimes a C is substituted for a G. Sometimes a few bases don’t get copied. Sometimes a sequence of a few bases gets copied in reverse order. That’s what genetic mutations are. Errors.
Sometimes the change, even of a single base, is enough to cause damage. The mutant gene—APC in colon cancer, for example—encodes a mutant protein that enables the single cell housing the mutation to grow at a faster pace than any of the cells surrounding it. At first, the change is minimal. But with cells growing and dividing more rapidly, the odds of another mutation are higher. So then one day, a cell with the APC mutation also gets a KRAS mutation, and now the dually mutated cells grow even faster. Soon enough, one of those cells gets a PIK3CA mutation, and now the cell is able to burrow into the colon walls, or find its way to a lymph node, or depart the mother ship for the liver.
It’s a matter of odds: The more cells you have, the greater the chance of a mistake, and the more mistakes that occur, the more likely it is that one of the mistakes will be harmful. Environmental influences may increase the likelihood of mutations. But so far, cigarette smoking, ultraviolet light exposure, and asbestos are among the few factors that are beyond debate.* The fact is that because cancer cells reproduce more rapidly than any other cell in the body, mutations occur in cancer cells in far greater numbers. Before long, the cancer cell is abnormal enough that it takes on behaviors that eventually kill us.
That’s cancer. That’s all it is. It’s the result of speeding up a perfectly normal bodily process. As George Johnson puts it in The Cancer Chronicles, “Cancer is not a disease. It is a phenomenon.”
And that is why cancer genomics matters: not because of the information, but because of what the information tells us about this disease, which is diagnosed in about 12.7 million people worldwide every year. Keeping up with the information for information’s sake is futile and pointless for most of us. But taken together, the findings call for a shift in our overall thinking about cancer. That change in perception matters when it comes to understanding why so many members of the human race, let alone one’s family, continue to die of cancer.
Yes, the specific abnormalities are interesting. Cancer is rife with darkly fascinating complexity. Some cases of myelodysplastic syndrome occur because certain genes, called tumor suppressors, are turned off through a process called methylation. That methylation pathway can be triggered by mutations in genes called TET2, DNMT3A, IDH1 or IDH2. That’s one of hundreds of such cases where the facts—the perpetrator, the weapon, the scene of the crime—are known.
But much of the time, there’s nothing else we can do with that knowledge. For nearly all the genetic mutations and resulting cellular mix-ups that have been chronicled, no drug exists to target that root cause. And not for lack of trying. Pharmaceutical companies have been attempting for years to make a drug to target the protein product of mutant KRAS, but no luck. Some targets are considered “undruggable”—maybe the shape of the errant protein is too flat or undulating for a drug to cling to. Sometimes the target is hit with a drug, but the rapidly mutating cancer finds a workaround before the tumor can be annihilated.
The great variety of cancers can also put a damper on things. Drugs that target driver mutations will work only in patients whose disease is guided by that driver mutation. Not all lung cancers are linked to ALK mutations, so the drug crizotinib, which inhibits the mutant enzyme, is prescribed only for that small subgroup of lung cancer patients. Identifying the driver mutations on which to focus treatment efforts is very difficult. For example, the APC gene can mutate several ways, and only one abnormality is responsible for driving cancer. The accumulation of new mutations as a tumor grows and metastasizes also complicates matters. Sorting through a tumor to find the causative mutants is like finding the tiniest of needles in a haystack where new needles keep appearing as the haystack grows.
The small patient population housing a particular driver mutation can be a pickle. Often the numbers are too small to obtain the meaningful statistics required to seek approval of a new drug. Also, the population might be too small to assure the drugmaker of a return on its investment. The expense and effort are increased by the FDA requirement that any company applying for approval of a drug targeted against a specific gene-driven abnormality must also produce a diagnostic test for that abnormality. After all, what’s the use of having a targeted drug if a patient can’t be tested for the target?
The integration of genetic information into patient care is having unexpected ramifications in the clinic. Sometimes, two patients with the same type of cancer may be dealt different prognoses depending on their genetic mutations. One leukemia patient but not another may be eligible for a bone marrow transplantation as a first line of treatment—a harsh, costly, but potentially curative treatment.
Looking at the long-term prognosis, considering the many mutations in a cancer cell, no single drug is going to stop a tumor from growing. Rather, patients will require a cocktail of targeted agents, perhaps in combinations that change throughout the course of the disease. But testing two experimental drugs in a clinical trial is forbidden, and even if it weren’t, it would be tricky to get two pharmaceutical companies to hop into human testing together. Gilead recently refused to continue testing its experimental hepatitis C virus drug in combination with one from Bristol-Myers Squibb, a match that resulted in stupendous results in early-stage trials.
Few researchers are throwing their hands up in frustration just yet, largely because of some standout successes. In 2001 imatinib was approved for the treatment of chronic myeloid leukemia, a disease that is almost universally caused by a single genetic mutation, known as the Philadelphia chromosome, and its resulting mutant protein. Ten years later, about 90 percent of patients taking the drug are alive and well (or died of other causes), a stunning outcome especially considering that the drug was nearly shelved during its development. (A story so extraordinary I wrote a book about it.)
So far, scientists have not found another cancer so clearly caused by a single mutation. For most malignancies, the story is much more complex, making treatments much harder to come by. It might be decades before the knowledge extracted from deep within a tumor is put to practical use. Years from now, it might be that when someone develops cancer, their doctor/biologist will sequence the tumor and offer up the diagnosis, not of colorectal cancer, but of an APC/KRAS/PIK3CA malignancy. A triple-combination regimen will be prescribed, pills that the patient can take at home. Every three months or so, the patient will return to get the tumor scanned again, and the drug regimen will be altered according to what mutations are now present.
That’s a tantalizing view of cancer that many clinicians consider reachable within our lifetime, and that, let’s be honest, may or may not come to fruition. On the way to finding that out, what’s the use of knowing anything about cancer genomics? No average person walking down the street needs to know what 41 genes are mutated in prostate cancer. But that person might want to know that cancer is a genetic disease. She might want to know that, at least according to science right now, there is nothing that a friend or relative could have done to stop the cancer from occurring. And she might simply want to wonder how something so deadly could come from the most fundamental structure of life.
*Correction, Oct. 22, 2013: This article originally stated that cigarette smoking is the only cancer-causing factor whose effect is beyond debate. (Return to the corrected sentence.)