A new study of fertility-clinic data is calling a major piece of conventional fertility-treatment wisdom into question. Among women younger than 38 who underwent in vitro fertilization in the U.S. in 2013, transferring multiple embryos did not result in significantly higher overall birthrates—just higher rates of twins, triplets, and other multiple births.
The study, published in this month’s issue of Fertility and Sterility, analyzed data collected in 2013 by the Centers for Disease Control and Prevention from 467 of the country’s fertility clinics. Researchers took into account the age of each patient, the stage at which each embryo was transferred, and the number of embryos each patient had available. Still, they found no significant difference in birth rates as the number of embryos transferred increased, though rates of multiples increased. “Cycle-level analysis found slightly higher live birth rates with double [embryo transfer], but this was mainly observed in women aged 35–37 years or with four or more embryos available for transfer,” the authors write.
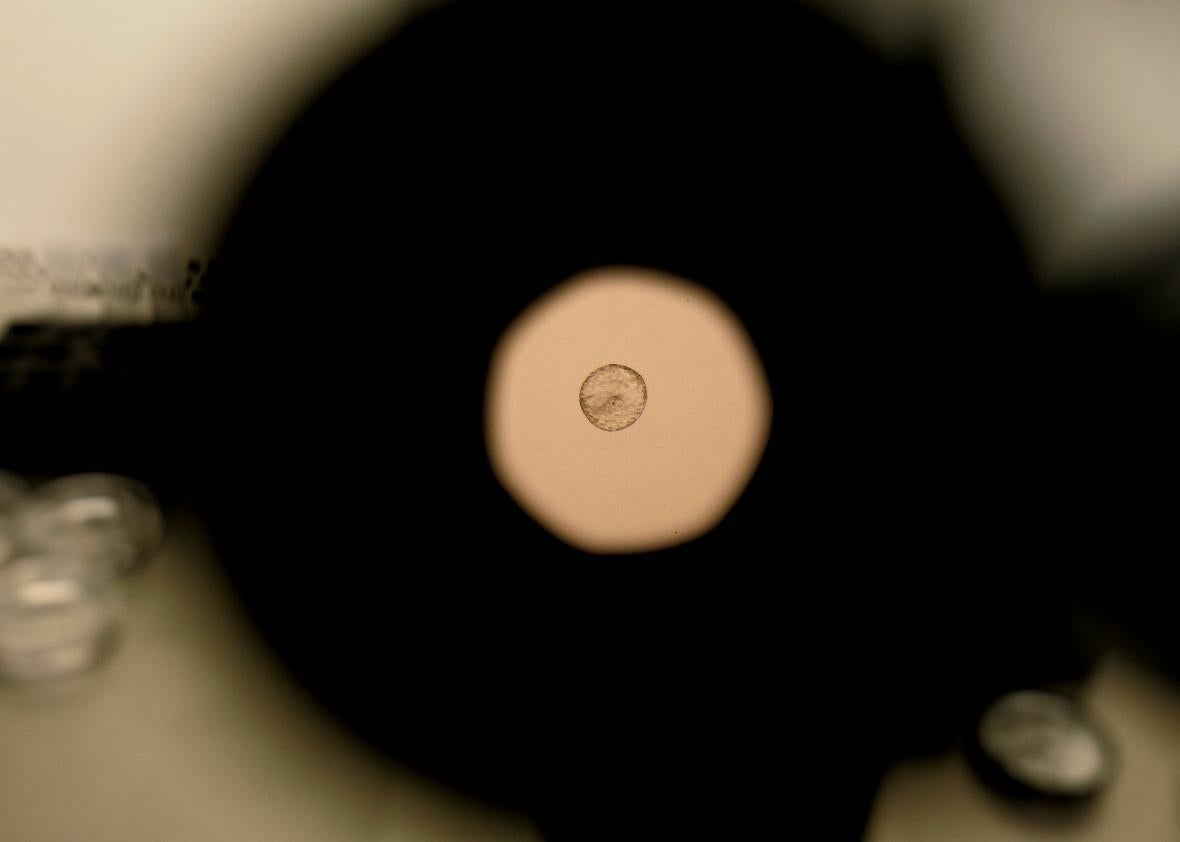
In 2013, the last year for which data is available, twins and other multiples comprised more than 41 percent of IVF deliveries in the U.S., the New York Times reports, because doctors often transfer two or more embryos at once to increase the odds of a successful pregnancy. Patients often choose this route to try to minimize the number of expensive, time-consuming, physically demanding IVF rounds they must complete, and doctors often urge multiple transfers to improve their clinics’ success rates. As a result, as IVF has grown in popularity and accessibility over the past few decades, the U.S. has seen a fast-growing number of multiple births.
Even though some people welcome multiples with excitement, they carry greater health risks than the average single-fetus pregnancy. Gestating multiple fetuses carries health risks for the both the pregnant woman and the fetuses. Women are more likely to experience miscarriage, pre-term delivery, gestational hypertension, postpartum hemorrhage, and preeclampsia; fetuses are more likely to be born at low birth weights, get tangled in their umbilical cords, and have underdeveloped organs or birth defects.
This is why, in August, the American College of Obstetricians and Gynecologists recommended that doctors “encourage and expand” transfers of single embryos. Even single embryos can split and become identical twins after transfer, but the risk of multiples is much, much lower with single transfers than with double or triple embryo transfers. Now, women under 38 might choose to minimize that risk, knowing they’re not halving their chances at a successful pregnancy by transferring one embryo at a time.