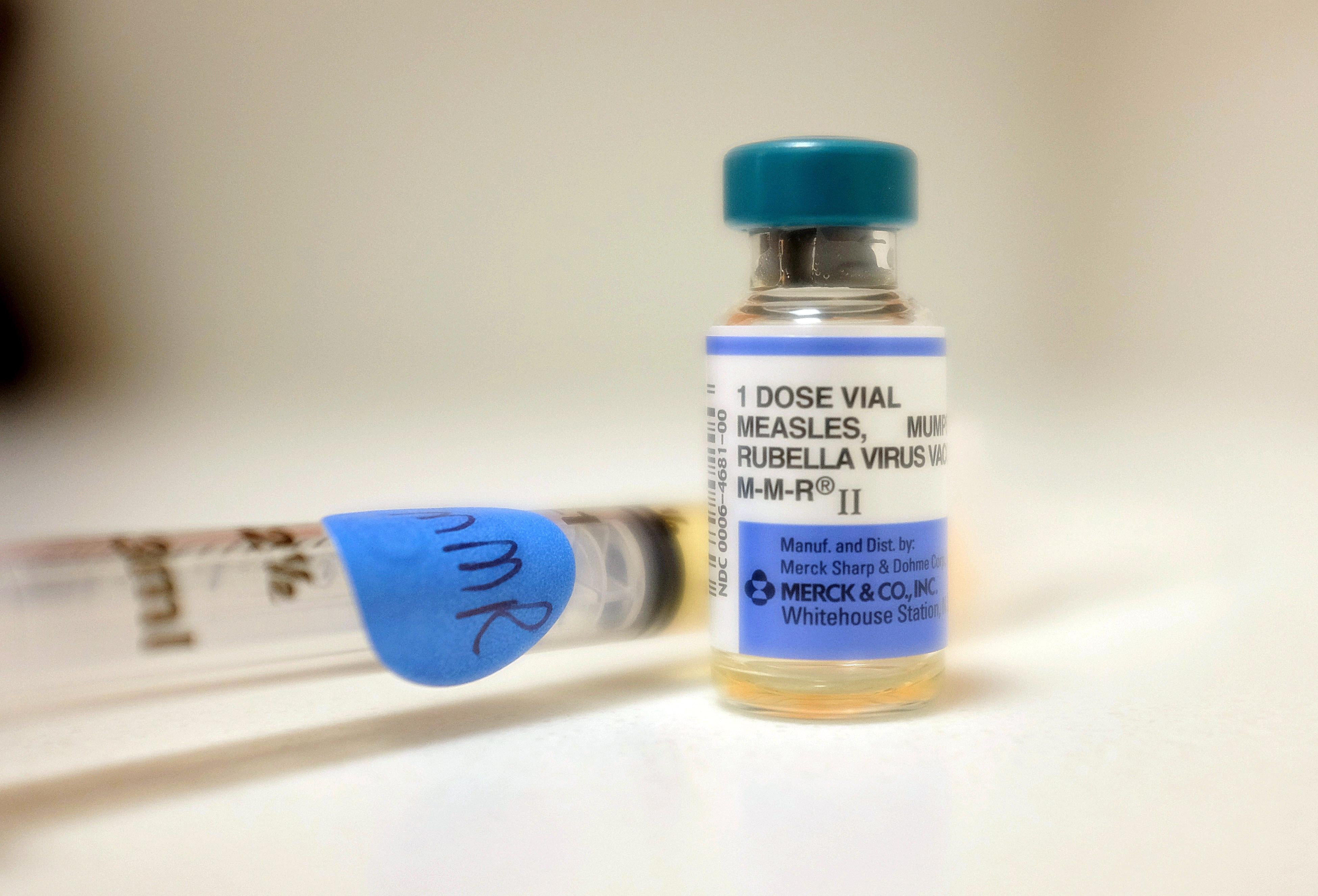
Since the beginning of June, there have been at least two big announcements about outbreaks of vaccine-preventable diseases in the U.S. this year. In California, more than 800 cases of whooping cough have been reported to the state health department in the past two weeks, according to Time. (Two infants have died from whooping cough in California already this year.) And on June 4, the Massachusetts Department of Health released a clinical measles alert to warn resident of a measles outbreak—nearly 300 cases in 18 states this year, with 89 percent of those cases in people who were not vaccinated. According to the New York Times, that’s a 20-year high.
If it seems like every month there’s a new outbreak of some preventable disease, that’s because there is. And yet, the anti-vaccine movement remains strong and intractable. I found out about the measles outbreak because someone posted the Massachusetts alert on Facebook, along with a plea to get your kid vaccinated because the original poster’s relative is an infant who has a disease that requires him to be on immunosuppressants. I reposted that message, but who knows if it did any good: As Amanda Marcotte noted in March, a study in the journal Pediatrics showed that pro-vaccine public health campaigns don’t really change minds, and in some scenarios make hardcore anti-vaxxers dig in their heels. So what does that mean for the rest of us? Should we just stop trying to convince the inconvincible and accept that we can’t slow down the spread of these preventable diseases?
Dr. Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, doesn’t buy the narrative of the unchangeable anti-vaxxer. He says there is actually a mushy middle of vaccine-hesitant people who are separate from the hardcore anti-vaxxers and estimates that of people who are delaying vaccines or foregoing them entirely, only 15 percent are unmovable. Other studies have shown that these “significant refusers” are only about 10 percent of the U.S. population. (Someone like Sara Pope, an anti-vaxxer who was on The Daily Show along with Dr. Offit earlier this year, will never be convinced no matter what the science says.)
So if that other 85 percent can be persuaded to vaccinate their children, what’s the best approach? Dr. William Schaffner, an infectious disease specialist at Vanderbilt University School of Medicine, says that pediatricians still have a lot of sway over the merely vaccine-hesitant. One way to persuade these parents to vaccinate, he says, is for pediatricians to get better training about how to deliver the vaccination message. That message should be “routine and strong,” Schaffner says, and doctors should be trained to answer common questions that might come up, rather than expressing exasperation at the first (or second or third) sign of reluctance.
As a larger public health question, as opposed to a doctor-patient relationship question, Offit believes fear-based messages are the most effective. The current generation of parents did not see peers get polio or mumps, so they’re not afraid of these diseases. But, “if we had a measles death”—which Offit believes is not out of the realm of possibility, because cases are on the rise—“it might change the tone of the conversation.” Some studies have, shown, though, that framing the message in a more positive way is more effective. A 2009 study from the Association of State and Territorial Health Officials found that the most compelling pro-vaccination message for parents is simply: “Vaccination is one of the most important ways I can protect my child.”
There is also a political piece of the puzzle, Schaffner points out, and a need for parents to advocate that states close their immunization requirement loopholes. There are currently 19 states that allow philosophical exemptions from school immunization requirements and 48 states that allow religious exemptions from those requirements. Washington, Oregon, and California have tightened their philosophical exemption policies for vaccines in the past few years, but they have not done away with them entirely.
On a national level, there is no well-funded organization exclusively dedicated to promoting better immunization practices, Schaffner says. He’s tried to drum up funding among pro-science philanthropic organizations “that could stimulate nonprofit groups to organize more effectively, but it simply isn’t there.” Hey, Mike Bloomberg: You took on the monster of climate change. Maybe you’re looking for another, less expensive pet cause?