During our Two Week Waits, my husband and I often take walks to the river near our house. Among couples trying to conceive (or TTC, as it’s known among people who have been trying for a while), the Two Week Wait is the wait between ovulation and a positive or negative pregnancy test. Online message boards are filled with advice about what to do during the Two Week Wait—go to the movies or out to dinner, take a yoga class, get a massage, anything to get your mind off the question of pregnancy. We have never been good at taking our minds off of anything.
We’ve also been TTC for long enough that we don’t expect a pregnancy, not really. For a while, particularly when we were treating our infertility with oral medications and intrauterine insemination, it seemed like every river walk involved a conversation about what if: What if this is the month? What if our child is born in January, February, March? The months fly by, 47 of them, and it’s time to make decisions about our next step.
Last month I did something different during the Two Week Wait: I visited an embryologist in her university laboratory. It has become clear to me, to my husband, and to our reproductive endocrinologist that IVF is the treatment most likely to overcome our infertility. But there are big questions: about the cost, about how we will feel if we try and fail, about the ethical considerations of spending so many resources creating a life that has not happened naturally, the way it does for most couples.
Even though IVF is still relatively uncommon—less than 5 percent of infertile couples are treated with IVF—everyone seems to have an opinion about it: what it does to the woman’s body, what one should do with leftover embryos, whether the treatment should be covered by insurance companies. Rational, loving friends and family have told me all kinds of unhelpful things: that a child I conceive through IVF will be more likely to have autism; that IVF will give me cancer; that I would be better off with acupuncture, herbs, or drinking more whole milk.
So it shouldn’t be surprising that politicians, too, are involved in the debate. In December, Personhood USA challenged Republican presidential candidates to sign a pledge to protect human life “at every stage of development.” This protection, if enacted through Personhood USA’s legislative proposals, would severely limit the practice of IVF. Five candidates—Rick Santorum, Michele Bachmann, Newt Gingrich, Ron Paul, and Rick Perry—signed the pledge, and Gingrich, a converted Catholic, expressed concerns specifically about IVF: “If you have in vitro fertilization you are creating life; therefore we should look seriously at what should the rules be for clinics that are doing that, because they are creating life.”
“I bet a lot of politicians have never stepped into an IVF clinic,” said Dr. Silvia Ramos, senior embryologist at the University of North Carolina School of Medicine, when I asked her about the personhood debate Gingrich was referencing. Born in Brazil, Dr. Ramos speaks with an accent that becomes more pronounced when she gets excited, and nearly everything about her work—from treating and interacting with patients to performing research on mouse ovaries and embryos—excites her. But about politicizing her lab, she is dismissive: “You need to have an understanding of science to know what goes on here. You need to have biological knowledge.”
My biological knowledge about embryo development was rusty, mostly comprised of half-remembered facts from health class, but Dr. Ramos patiently and enthusiastically described the process of IVF, which begins when she receives the eggs retrieved from a woman’s ovaries by the reproductive endocrinologist. In a sterile laboratory, she observes each egg, or oocyte, under a microscope and determines if it is mature enough for fertilization. If the patient has chosen intracytoplasmic sperm injection, a procedure designed to overcome male infertility, Ramos will carefully remove the cloudy masses of nurse cells surrounding each mature oocyte, and will inject the oocyte with a single sperm selected for optimum morphology and motility. This process can take an hour or more, and often she will listen to Brazilian bossa nova CDs as she works. “You have to be in peace every day to do your best at this,” Ramos said. “Music helps.”
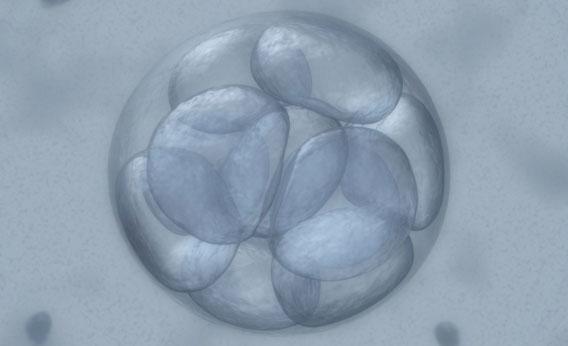
After so many months of TTC, I found Ramos’s step-by-step description soothing, even appealing, for its order and predictability, for the way it makes conception—that long-elusive goal—visible. If the oocyte is fertilized, Ramos will see the formation of two pronuclei, then the fusion of the diploid cell, or zygote. Over the next few days, as the zygote is incubated at 98.6 degrees, she will track its development in the lab. Ideally, the zygote will form four even, smooth cells, then eight. Sometimes, Ramos can wait for the embryo to become a morula, which looks like a blackberry, or a blastula, which looks like a soccer ball, before transferring the embryo to the woman’s uterus. “Look! How beautiful!” Ramos said, showing me images of embryos she had worked with. She had folders and folders full of these images, and they were, at every stage, strangely beautiful, as were her tools: the polished steel and glass pipet used to move the embryos, the tiny, needlelike cryoloop used to cryopreserve the leftover embryos using vitrification.
“What happens here in my laboratory is a lot like what happens in the woman’s body,” said Ramos. “No one sees it.”
Except they do. The day of transfer to the uterus Ramos gives each couple or individual a set of images of their embryo or embryos, plus a description of the embryos’ condition and likelihood of implantation. I can imagine that these blobby, black-and-white images are precious to anyone who has experienced years of trying. Women on TTC message boards, women with screen names like Babybound or Tryn2BMommy, will send each other “sticky vibes” or “baby dust” in the hope the embryos will “take.”
But in the clinic they practice a cautious optimism. Sometimes patients cry, Ramos said, but they never name or otherwise personify the embryos. There are too many things that can go wrong—the embryos, still months from viability, may not implant, or they may implant but stop developing. Extra embryos are frozen, and patients at UNC have three options: They can store the embryos for future tries, they can donate them for research purposes, or they can destroy them. Destruction of a stored embryo is accomplished by thawing. “The embryos belong to the parents,” said Ramos. “They have the right to decide.”
And they are the ones who know, ultimately, the impact and import of IVF, a treatment that is so expensive, invasive, and fraught that it is rarely—if ever—begun lightly or heedlessly. Dr. Ramos often has to call her patients to give them disappointing, even devastating, news: embryos, especially those from the oocytes of older women, sometimes have fragments or stop developing, and it is difficult to tell which ones will implant successfully. Despite this uncertainty, Ramos’s discussion of IVF was punctuated by frequent, enthusiastic exclamations about the great love she has for her job. “It’s so delicate,” she said. “It takes the right combination of skill and personality to do it well. I create life. This is what is magic.”
I looked up from the notebook where I’d been writing and sketching zygotes—did she say she creates life?—but then Ramos went on to talk about the life of the family: mothers and fathers and children, or mothers and mothers, or fathers and fathers, birthdays and holidays, traditions passed on, one generation to another. That is the life she helps create, the life she or another embryologist offers me and my husband.
Near the end of my visit, our conversation turned from the theoretical consideration of morulas and blastulas to the specific realities of my own condition and treatment. Very politely, Dr. Ramos asked my age, and I told her. “Now is your time,” she said.
She is probably right. Our two-week wait is over, and—as I have come to expect—we are still TTC. Visiting Dr. Ramos did not answer my questions about money or the use of resources or the exposure to heartbreak. But in my waiting moments, in the space of what if, I can picture myself receiving a phone call from her. “Beautiful embryos,” I picture her saying, a bossa nova melody playing in the background. I picture the embryos themselves: round blastulas, with evenly divided cells.
Though even then, we would still be waiting.
***
My doctor sent me an email about waiting. The word obstetrician, wrote Dr. Young, has as its Latin morphemes ob, which means across, and stare, which means to stand. An obstetrician is someone who stands across from his patient, waiting to bring forth her child. (And then there is that word, patient, and all that it implies.)
Dr. Young waits, too, but not in the same way. He practices not as an obstetrician but as a reproductive endocrinologist, a doctor who diagnoses and treats long periods of waiting, and who waits for women like me—waffling, indecisive, fearful—to decide what to do. When his patients become and stay pregnant, they eventually “graduate” to an obstetrician, who will be the one to deliver their babies. Dr. Young waits for the correct combination of treatments to take effect—he waits, like us, for the pregnancy.
I have been diagnosed by Dr. Young with a luteal phase defect, meaning that my endometrium, my uterine lining, does not wait long enough before shedding each month. This has been treated through progesterone supplements, which I take after ovulation. My cycle is now a regular 28 days; my endometrium waits properly—two full weeks—for the blastula to implant.
Except that it doesn’t. I have never been pregnant—at least, I have never confirmed a pregnancy through a positive E.P.T. or First Response testing kit. In fact, I have taken very few pregnancy tests in my years of reproductive maturity—once when my husband and I were living in Brooklyn, and three times in the 47 months we’ve been trying. I take my temperature every morning, and usually, near the end of my cycle, I will see a pattern of falling temperatures—98.5, 98.3, 98.2—that tells me the Two Week Wait is nearly over.
In this way I’m unusual. On message boards and in the support group I attend, TTC women talk about testing daily, even twice a day, during their Two Week Wait. Sometimes they are waiting for a positive result—usually, the soonest that home pregnancy tests can detect hCG in a woman’s urine is 10 days past ovulation—but other times they are confirming and reconfirming a positive result. I’ve heard of women taking two or three tests to prove—to celebrate?—what one test showed: the dark line, the plus sign, the word pregnant.
I can well understand that this is soothing to them, comforting in the same way that Dr. Ramos’ evenly dividing embryo cells were to me. Because the embryo and the changes to the body are longed-for, expected, and (at this point) invisible, TTC women desire anything that makes the pregnancy seem “real.” Of course, she might not share this information publicly—most agree that waiting until the end of the first trimester is wise—but among her TTC associates, other women who are waiting to hear the results of her treatment, she will probably share. Online, such news might be delivered through an exultation—“Yippee!!! BFP!” (Big Fat Positive)—or an image: a photograph of the home pregnancy test, or a smiley-faced icon of a pregnant woman holding her rounded belly.
Infertility and assisted reproduction can be difficult to talk about with fertile people—they may not understand, may not want to talk about it, or may be too busy raising their own families to offer much support. A message board or blog is a safe place to talk about injectable medications, IVF cycles, or the question that plagues every Two Week Waiter, no many how many movies she’s seen or yoga classes she’s attended: Am I pregnant—or not? Though mediated through a computer, the support offered by women on these boards is conversational—filled with sentence fragments, terms of endearment, urgent questions, and exuberant punctuation. Their messages are decorated with animated GIFs that are like body language or gesture in a face-to-face conversation: cartwheeling or cheerleading smiley faces, illuminated BFPs, shimmering baby dust.
On the website Lilypie.com, a TTC woman can create a custom ticker—a colorful graphic image that counts up or down—to appear below her posts to infertility and assisted-reproduction message boards. As I visit these boards, I often see, below a list of relevant details—ages, medical conditions, number of months or years TTC, the dates and results of various IUI or IVF cycles—these small, rectangular banners, frequently more up-to-date than the posts themselves.
Tickers can provide a digital reminder of all kinds of things—vacations, anniversaries, birthdays, and graduations are all popular events to anticipate via ticker—but they have a particular significance and prevalence in the infertility community, where conception and pregnancy are marked by a series of emotionally fraught, unseen events that might be shared only in anonymous places like Internet message boards. Like medieval manuscripts, the tickers are illuminated with images that represent the text, pastel pictures you might see on any baby shower invitation: infant clothes, a pram, smiling cartoon storks. On Lilypie, you can choose to mark a menstrual cycle from 15 to 80 days long, using a variety of backgrounds: butterflies, the city at night, a cabbage patch, or stars. (Fertile days in a cycle might be marked with hearts or a sprinkling of baby dust.) The “slider” is the image that will mark where you are in the cycle, and it’s customizable, too; choices include a gleeful rabbit, a woman jumping through a hoop, or a variety of cartoon pairings: bees, ladybugs, a man and a woman holding hands, two women holding hands, or even two men holding hands (presumably, they are marking a surrogate’s cycle).
There are also “angel baby” memorial tickers for children lost to miscarriage or stillbirth. Backgrounds include clouds, rainbows, and serene meadows, and sliders include doves, teddy bears, bunnies, and babies of various ethnicities and postures: some are sleeping peacefully, while others are sitting upright and haloed, heaven-bound. Some have wings, some slide down rainbows; they come in singles or groups of two, three, or four. They all look the way we expect babies, not embryos or fetuses, to look; they are pleasantly chubby, adorably forelocked, dressed in shades of blue or pink. The suggested message for an angel baby ticker is “It’s been x months & y days since we said goodbye.” The grieving mother might have lost her baby at birth or sometime long before—in IVF, losses are common days or weeks after the transfer of embryos. Though books might tell her that her baby, at three to four weeks, is the size of a poppyseed, that is not what she pictures. She imagines a “real” baby: smiling, gendered, and cuddly. But the angel baby—a cartoon, an image, an idea—might be all she gets.
Before we had the technology we have now—before home pregnancy tests, before IVF, before microscopic images of blastulas—a pregnancy was suspected with a missed period, but imminent life was confirmed not through a visual sign but through the quickening, the first fetal movements felt by the mother, which typically happens at four or five months’ gestation. Aristotle considered quickening the signal that a human soul had entered the fetus. Until about 100 years ago, when doctors and scientists began collecting and displaying fetal specimens, most people could not picture an embryo or a fetus—and didn’t try. In some cultures, fetuses born very prematurely were so foreign and unfamiliar that they were interpreted as something other than human—as kangaroos, monkeys, fish bellies, or spirits.
It is now possible, in the most advanced and high-tech RE clinics, to record every moment of cell division in an IVF cycle through time-lapse imaging. Embryologists believe that by studying these images—how and when each embryo divides—they will be able to select the best-quality embryos for transfer, improving the patient’s likelihood of pregnancy. Such images will surely become the subject of political and bioethical debates—the time-stamped creation of life is a powerful tool for those concerned with personhood at the cellular level. Dr. Ramos, for her part, is excited by the extra assurance this technology offers her patients and hopes to obtain it for her laboratory in the next few years. By then, my decision will be made. I will have tried IVF. Or I will have moved on.
***
I told a friend recently that sometimes I feel strangely grateful for the pause I’m in now. My husband and I both know it is unlikely that natural TTC cycles will produce a pregnancy for us, and we have time—a little bit, anyway—to consider not only the financial and emotional cost of an IVF cycle or cycles, but also how a pregnancy would affect our lives. Our house is 800 square feet, for example. Where would we put the crib? When would I write, and who would take care of our child while I teach or my husband works? What if the child is sick or troubled; what if I am a bad mother? What if?
My friend, childless herself, and a biologist, said she thought it was better when you didn’t try to answer those questions first, when a pregnancy made the answers irrelevant. I agree, and I would trade these questions and reservations in a second for a pregnancy that happened without medical intervention. But that isn’t my situation, and it probably won’t be. So I have to ask the questions. I have to visit the clinics and the labs, talk to the doctors, read the message boards, walk to the river with my husband. I have to talk about uncertainty and ambivalence with my child-free friends, the writers and artists and scientists I know who are making a life that is not organized around childrearing.
But I’ve decided I like the word pause better than the word wait. Sometimes it’s used as a euphemism for menopause—and I hope that is years away—but I interpret pause not to mean the suspension of all activity, but the cessation of frenzy and anxiety. It implies peace and freedom, reflection, even agency, in a way that wait does not. The recently published book Bringing Up Bebe uses the word to describe the way a French parent takes a moment before comforting a crying child. The pause gives children an opportunity to self-soothe, to calm themselves independently instead of relying on an outside force. If I ever have a child, I will surely try this parenting trick, but for now, it seems to apply to my own life. I think of the interests I have—writing, reading, listening to music, kayaking—all as self-soothing exercises, as forms of independence from suffering, from sadness, from focusing too hard on the wait. They are also the life, at the moment, that is most visible and real for me.