Masayo Takahashi is at the Riken Center for Developmental Biology in Kobe, Japan, where she heads the Laboratory for Retinal Regeneration and is planning a pilot safety study using a type of stem cell to treat age-related blindness.
Natasha Little: Later this year, you will make history when you begin the first ever human trial of induced pluripotent stem cells. Why is this such a big deal?
Masayo Takahashi: Stem cells have enormous medical potential because they can become any other type of cell. If we can use them to replace old or damaged cells, this could have huge implications for treating degenerative diseases.
Stem cells can be harvested from embryos, but this is ethically controversial. Despite this, there are several trials of these embryonic stem cells underway. Their use often requires drugs to stop the immune system from rejecting them, which can cause complications for elderly patients. Induced pluripotent stem (iPS) cells offer an alternative. These are made from a patient’s own cells, removing the need for the immunosuppressant drugs. Plus there are no ethical issues.
NL: How would treatment with iPS cells work?
MT: The iPS cells are made by injecting several “reprogramming” genes into adult cells that have been removed from the body. This makes them rewind to an embryonic state. Then we can make iPS cells differentiate into the cell type we need by injecting proteins that instruct embryonic stem cells to become liver, retina, or any other type of cell. The idea is that these reprogrammed cells can then be inserted in the body to replace damaged cells. We are at least 20 years from any clinical treatments, but the potential is exciting.
NL: Are there any potential pitfalls with iPS cell treatments?
MT: Yes, we have to be very careful because iPS cells multiply endlessly. This means that if any undifferentiated iPS cells were accidentally put into someone, they could cause tumors. That’s why this study is so important. It is not a clinical trial, but a six-subject pilot study to confirm the safety of putting cells derived from iPS cells into humans.
NL: Who are the participants in the study?
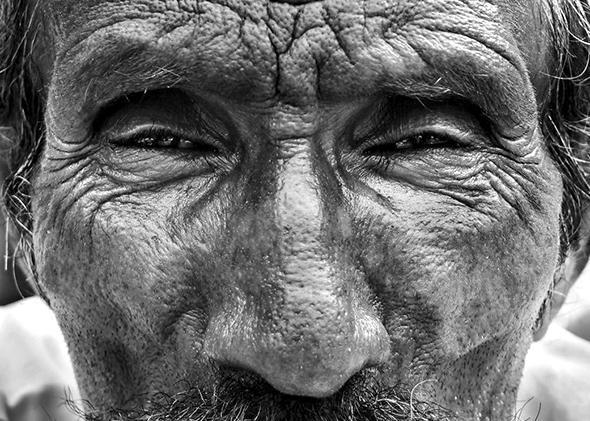
MT: The six people all have age-related macular degeneration in their eyes. This weakens the vision in the central field, eventually leaving people with only peripheral vision. In the type of degeneration we are working with, this is caused by the deterioration of the retinal pigment epithelium (RPE)—the layer of cells that clears away extracellular debris that lands on the retina.
We aim to replace the damaged section of the RPE with cells created from skin taken from the patient’s arm. The skin cells will be reprogrammed into iPS cells and then differentiated into RPE cells. It will take a year to grow enough RPE cells to introduce them to a damaged eye. Although I am excited to see if there is any improvement in sight, this study aims only to demonstrate the safety of RPE cells derived from iPS cells.
NL: How confident are you that the pilot will be a success?
MT: Very confident. We have trialed this intervention on mice, rats, and monkeys and observed no tumors. I chose to work with RPE cells because of their characteristic brown pigment. This means we can avoid injecting tumor-causing iPS cells by selecting only the clumps of pure brown RPE cells. Of course, we do have to pick out around 50,000 RPE cells, so it can be a bit tough.
Another reason for optimism is that the retina is the safest place to try this out because we can watch the cells closely through the participant’s dilated pupil.
NL: What does the future hold for iPS cells?
MT: Right now it takes a lot of time, money, and labor to reprogram cells. In our study, each intervention costs 20 million yen ($200,000) per eye and will take 10 people a year to complete. However, my research uses “auto-transplantation,” in which the iPS cells come from the patient. The possibility of “allogeneic” treatment, in which iPS cells from one person could be used in many people, could reduce the cost tenfold. Shinya Yamanaka [who won a Nobel prize in 2012 with John Gurdon for discovering iPS cells] plans to create an iPS cell bank to store a number of genetically average iPS cell cultures—those that most easily integrate into people without immuno-rejection.
The greatest barrier to iPS cells being used to treat diseases of other organs is the difficulty of growing large quantities of cells. The retina only needs one dish of cells. To replace part of the liver or hip would require thousands of times as many.
However, there is no doubt this is a very exciting area with huge potential. My husband, Jun Takahashi, is planning on carrying out a safety trial of a treatment for Parkinson’s disease based on iPS cells in two years time. I don’t know if he can do it, but he says he can.
NL: How important is the discovery announced this week that any adult cell can be rapidly reprogrammed just by putting it in a bath of acid?
MT: The work is very exciting and will change many aspects of regenerative medicine in the future. I am looking forward to seeing where Haruku Obokata’s [who carried out the work] research leads. I feel joyful that we are both working in this wonderful area of science.
This article originally appeared in New Scientist.