What did you do on your summer vacation? I got a new kidney. Actually, it is my second. The first transplant, which I received in 2006 from a once-distant-but-now-dear friend, Virginia, wore out earlier than expected—I’d hoped to have it for 20 years. This one was from a solid-but-not-best-but-now-beloved friend, Kim, who had considered donating when I first became ill and was recently able to do so.
I am almost obscenely lucky. Within a 10-year period, two glorious women rescued me from years of grueling dialysis and a guarantee of premature death. After my first transplant, Kim had told me that she would be willing to donate to me if I needed another kidney. (While most cadaver kidneys typically last 10–12 years, living donor kidneys tend to last 15–20 years. Mine started to give out early, sadly, so I knew I would need another sooner than later.) It was Kim, not I, who raised the offer whenever we got together on her trips east from her home on Bainbridge Island in Washington state. Her tremendous generosity allowed me to live many years in peace instead of constant worry.
Finding a donor the first time around was a nightmare, however. I learned I had pending renal failure during a routine check-up in the summer of 2004. It’s not clear why my kidneys gave out. But the fact that I felt pretty well at the time of diagnosis suggests this was not an acute development but rather the result of silent loss of function that had been in progress for at least a decade.
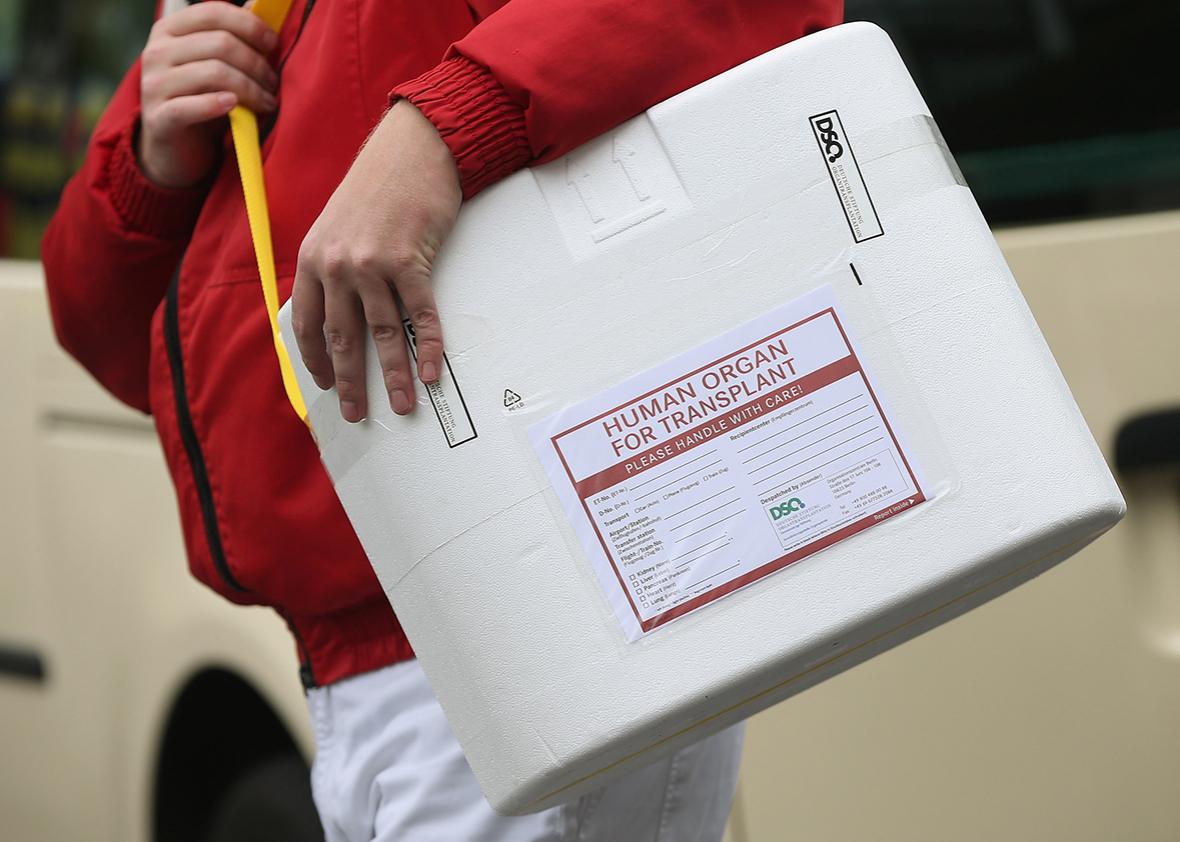
I knew from my medical training (I’m a psychiatrist) that I needed to start looking for a donor soon. A living donor is the ideal since those kidneys last longer. Also a cadaver kidney usually takes years to acquire from The List (the national transplant queue overseen by the United Network for Organ Sharing). The wait would require me to go on dialysis, and transplants, whether from living or posthumous donors, don’t last as long in people who have been on dialysis first.
So, I soon found myself in the business of hinting to friends—I never quite asked outright—that I would be very grateful indeed if they would just consider taking on the small-to-modest risk of giving me a body part. Not an easy conversation, but necessary. Unsurprisingly, many people struggle with how to respond and so next came a soul-crushing succession of unfulfilled promises, disappearing acts, and cold feet. I even had an almost-promised kidney rescinded after someone else interfered. And as anyone who’s been there knows, all of these blows must be weathered in a gracious and upbeat manner.
Still, I understood the general reluctance to donate. After all, giving a kidney is by no means risk-free (roughly a 0.02 percent, or 2 in 10,000 mortality rate, a 3–5 percent rate of serious complications, and perhaps a 25 percent chance of minor complications). Also, some people want to “save” their kidney lest, say, their own child needs it. Then, too, a lot of people are simply put off by surgery, and some handful—no one knows the extent of this group—can’t afford time off and lost wages.
Of the 120,000 people waiting for organs, 101,000 are waiting for kidneys. That is largely because patients with renal failure can exist for years on government-funded dialysis: Patients with, say, liver and lung failure die relatively quickly without a transplant. Most organs come from deceased donors anyway, but it’s clear that friends and relatives are not lining up to give the “gift of life.”
So thank God for Virginia, who, upon hearing from a mutual acquaintance in the fall of 2005 that I needed a kidney, emailed me right away: “If I am a match, I will do it.” And, again, blessings to Kim who kept her kidney warm until I needed it this summer. My transplants were a matter of private policy. My friends saved me—out of empathy, out of principle, out of affection. I’m beyond fortunate for them, because our public policy is failing far too many people who need organs. Twenty-two people die each day because they cannot survive the wait for an organ; 12 of those die from lack of a kidney in particular.
The core of the problem is that prospective donors are legally required to relinquish an organ in the spirit of “altruism.” Despite the risk they take on, they are not allowed to benefit materially in any way. This mandate is part of the 1984 National Organ Transplant Act, the law that established the national system of organ procurement and distribution. Any exchange of an organ for any sort of “valuable consideration,” is a felony punishable by up to five years in prison and/or a $50,000 fine.
The original law was intended in good faith. The point was to prevent a classic free market where only wealthier patients could afford to buy organs; it also sought to avert the scenario where poor donors were the “suppliers” for the well-off. Understandably, legislators wanted to give an altruistic system a chance to work. But more than enough time has now elapsed to conclude with certainty that an altruism-only system is sorely inadequate. And as in so many realms, it is the poor (especially poor minorities) that have suffered the most because of the deficit. They are less likely to be referred for transplant, more likely to die on dialysis, and less likely to receive an organ from the national pool even when they are referred.
For decades now, the transplant community has mounted educational efforts, improved its procurement efforts at the time of death of potential donors, and so on. Yet, the number of donors each year, living and deceased combined, remains mostly flat. There has been a relatively recent growth in so-called organ “swaps and chains.” A swap is when willing donors don’t match with their intended recipients, so donors are swapped to make a match and both patients end up with a kidney. A chain is essentially a series of swaps, but the logistics involved in setting one up is very complicated. Last year, swaps and chains combined accounted for roughly 550 transplants—an exciting innovation but a modest one given the total number of people in need.
It is clear that a new policy is imperative, and fortunately one could soon be on its way. In May, Pennsylvania Rep. Matt Cartwright introduced a bill called the Organ Donor Clarification Act of 2016. Its goal is to permit study of the effect of rewarding people who are willing to save the life of a stranger through living donation: Not through a free market with direct cash payments, which would bring up insurmountable ethical concerns, but through other regulated and limited means. The bill establishes that five-year pilot studies could be conducted without breaking the 1984 law, so long as they pass ethical scrutiny by an independent board under auspices of the Department of Health and Human Services.
The pilots would test how various rewards resonate. Rather than large sums of cash, potential rewards could include a contribution to the donor’s retirement fund, an income tax credit or a tuition voucher, lifetime health insurance, a contribution to a charity of the donor’s choice, or loan forgiveness. Only the government, or a government-designated charity, would be allowed to distribute these benefits. (The funds could potentially come from the savings of stopping dialysis, which costs roughly $80,000 a year per person.) In other words, needy patients would receive kidneys regardless of their ability to reward donors out of their own pockets.
The pilot programs, to be designed by individual medical centers, could also impose a waiting period of at least six months before people can donate, thereby ensuring that they won’t act impulsively and that they give fully informed consent. Prospective donors would be carefully screened for physical and emotional health, as all noncompensated kidney donors are now. These arrangements would filter out financially desperate individuals who might rush to donate an organ in exchange for a large sum of instant cash and later regret it.
The donors’ kidneys would be distributed to people on the waiting list according to the rules now in place. Finally, all rewarded donors would be guaranteed follow-up medical care for any delayed onset complications—bizarrely something that is not currently the case, though it should be.
The Cartwright bill is a very modest measure that simply allows medical centers to design and implement these trials to see if they work. It would not provide any funding; the medical centers would need to obtain that themselves. But the bill is a bold challenge to the longstanding ethos of the transplant culture: the reflexive insistence that donors not be enriched for their noble sacrifice. Cartwright’s proposal is the most realistic policy idea out there—if it wins support and is implemented. We’ll see what happens when Congress votes on it.
I was truly blessed to have Virginia and Kim, for whom giving the gift of life was reward enough. But there is no reason we should maintain such a high burden when there are ethical alternatives, and when the cost of not using them is so high. A truly responsive public transplant policy must expand beyond the “gift of life” sentimentality to accommodate potential donors who would like to benefit in return for saving a life.