On a sunny June day in 2014, I returned home from a walk in my neighborhood with what I thought were mosquito bites on my leg. Most of them quickly faded away, but one, with a tiny black dot at its center, did not. It grew. After days of denial, I dragged myself into the doctor’s office, where I was told it was probably a MRSA infection and sent home with a prescription for antibiotics and with a lot of fear.
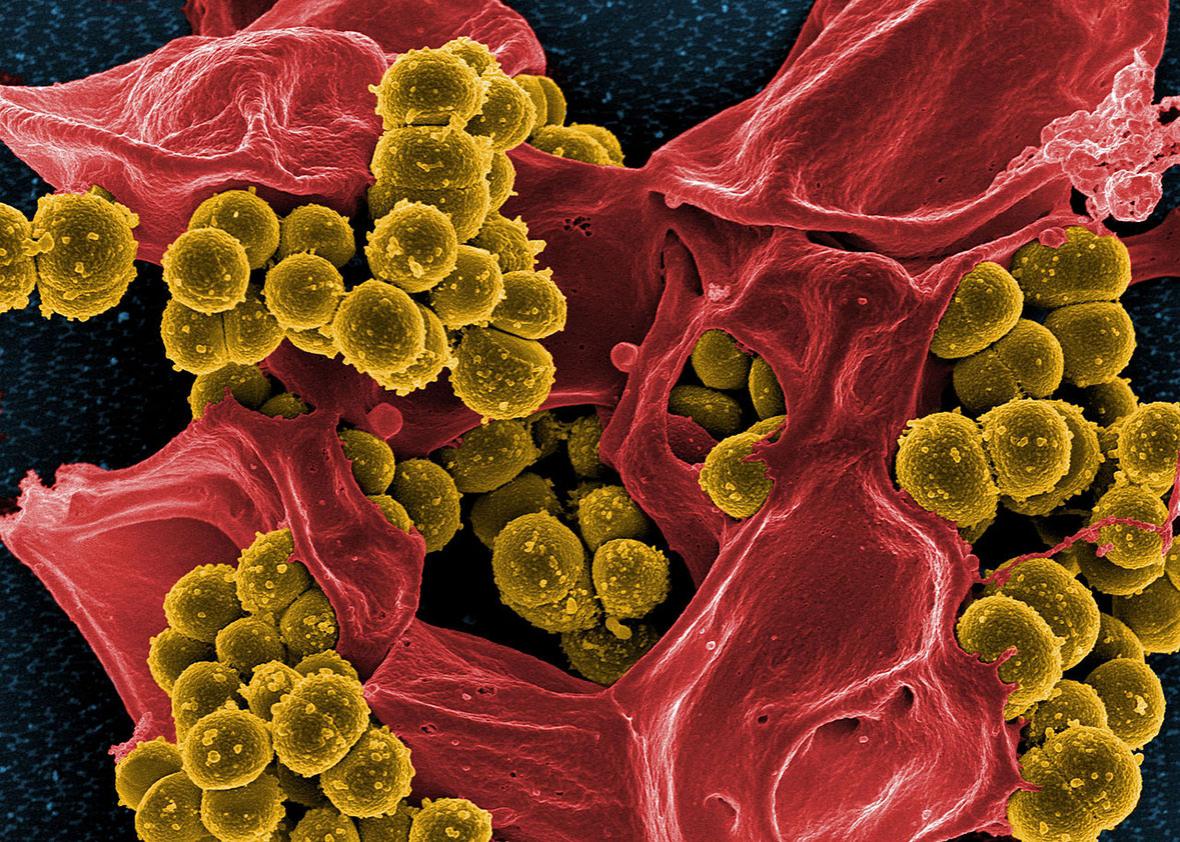
MRSA stands for methicillin-resistant Staphylococcus aureus. Staph is a widespread and usually harmless bacterium; about a third of people carry staph in their nose, a major reservoir for the bacteria. When staph does cause an infection, antibiotics should clear it up. But that becomes more difficult with MRSA strains of staph, which can’t be killed by penicillin, methicillin, or related antibiotics. MRSA strains can be deadly, killing thousands of people in the United States every year. I couldn’t help but wonder: Would I be one of them?
To make matters worse, I was editing a two-part story on antibiotic-resistant “superbugs,” so I couldn’t get away from the scary stats. The World Health Organization had warned that antibiotic resistance had reached “alarming levels,” the story said. A WHO survey had found that in some countries, antibiotics no longer worked for half of the people infected with common diseases like bacterial pneumonia. The Centers for Disease Control and Prevention estimates that 2 million people in the United States contract antibiotic-resistant diseases every year, and some 23,000 die from these infections.
Experts have warned that we may be headed for a “post-antibiotic era” in which the drugs no longer work. The drugs have been a literal lifesaver for millions of people, contributing to a dramatic increase in lifespan in the past century. A future without them is absolutely terrifying. A bout of strep throat, an ear infection, or even a cut on your finger could be deadly. Medical treatments that now save people—from chemotherapy to transplants to surgery to dialysis—would bring such a risk of infection that it might be too dangerous to perform them.
I got a prescription for an antibiotic that MRSA is not supposed to be resistant to, but it didn’t help, and my infection continued to spread. The solution: cut the infection out, a procedure that took only a few minutes and left me with a hole in my skin just below my right knee. (I’ve since discovered this was what should have been done in the first place.) Lab tests later confirmed that it was MRSA.
MRSA first showed up in the United Kingdom in 1961, shortly after methicillin was introduced, and it soon spread around the world. Infections at that time centered around hospitals, where the bacteria flourished among a vulnerable patient population. By the 1990s, MRSA was endemic in large university hospitals and intensive care units in the United States. But until then, the bacteria rarely infected anyone who was healthy.
I often get asked where I picked up MRSA and whether I had been to a hospital in the days before my infection. “No,” I tell them, “not for years.” Around the time MRSA rooted itself in our hospitals, it also escaped from them, creating a new problem known as community-associated MRSA.
Football fans may be familiar with CA-MRSA. New York Giants tight end Daniel Fells has been battling a MRSA infection on his ankle this fall, and his doctors were worried they might have to amputate his foot. MRSA outbreaks have become distressingly common among athletes, both amateur and professional, and especially in sports where skin-to-skin contact occurs. But scientists don’t yet know whether it’s the contact with each other, the field, the equipment or locker rooms, or something else that makes athletes prone to these infections.
And it’s not just athletes who are at high risk. MRSA appears to spread easily in places like military barracks and prisons. And certain populations may be more vulnerable, including children, native Hawaiians and Alaskans, and anyone in a household where someone has had MRSA. There are even indications that owning a pet may put someone at greater risk of infection.
But the truth is that MRSA has become so widespread that anyone can now become infected, even an otherwise healthy adult like myself. And I didn’t need to go anywhere special to pick it up. Scientists have found MRSA lingering on the seatbacks of airplanes, in meat from the supermarket, in coastal waters, and possibly even in the wind. Two percent of people harbor MRSA in their nose. Superbugs are everywhere.
Bacteria like S. aureus gain resistance to antibiotics because they have the capability to evolve quickly, and any bacteria that withstand the drugs outcompete those that can’t. But we are not doomed to an antibiotic-free future, Robert Daum, head of the MRSA Research Center at the University of Chicago Medicine, told me. Staying ahead of evolution requires a three-pronged approach: developing new vaccines against bacteria like S. aureus, developing new antibiotics, and making better use of the ones we have.
A vaccine against MRSA is currently in development. The National Institutes of Health has sponsored an initiative to design and conduct clinical studies that reduce the threat of antibiotic resistance, and developing new antibiotics is one of the goals. And the CDC is working with pediatricians and other doctors to reduce antibiotic use to slow the development of new resistant strains of bacteria.
Overuse of antibiotics remains a huge problem, however. The CDC has estimated that half of antibiotic prescriptions are unnecessary. Antibiotics are often used against viral infections like the cold and flu—even though antibiotics don’t kill viruses. Every time someone takes an antibiotic for a viral infection, not only will the drug be completely useless and possibly have harmful side effects, but it may also help induce resistance in previously harmless bacteria.
An even bigger problem is in agriculture, where about 80 percent of antibiotics administered in the United States are used. Most farm animals that receive antibiotics aren’t even sick; the drugs are given to animals to make them grow faster with less food. And while the Food and Drug Administration recently released voluntary guidelines to reduce antibiotic use in livestock, there are gaps that may allow for overuse. And the danger here isn’t theoretical. Scientists have traced a strain of MRSA carried by livestock to patients in British hospitals.
I recovered from my bout with MRSA with a small scar to remind me of the experience, an apartment laced with the bacteria, and a 50 percent chance of getting infected again. And I am concerned that I may accidentally pass the bacteria on to someone who doesn’t have as robust an immune system—a friend battling cancer or a relative recovering from a transplant, for instance—or someone who doesn’t have good access to health care.
In the end, though, I got off lucky. The MRSA infection wasn’t even the worst part of what happened to me. (Remember that antibiotic I’d been prescribed that didn’t work? It turns out I was allergic to it, which I discovered when I woke up one day with a fever and full-body rash.)
But what’s really frustrating is that this didn’t have to happen. The rise of antibiotic resistance wasn’t a surprise. Alexander Fleming, in accepting his Nobel Prize in Physiology or Medicine in 1945 for discovering penicillin, warned that it was likely to occur. So while it’s great that the problem is getting attention, that WHO declared a World Antibiotic Awareness Week this month and the White House released a national plan for combating antibiotic resistance, overuse of antibiotics is still rampant. Which will evolve faster: microbes or people’s ability to fight microbes? We must slow bacterial evolution enough to save these miracle drugs so they keep saving lives for generations to come.