The plight of Sarah Murnaghan made headlines over the past several weeks. The 10-year-old girl suffers from cystic fibrosis, a crippling respiratory ailment. She was dying, but she was deemed ineligible—then, after an uproar, eligible—for an adult lung transplant. She received a new set of lungs on June 12.
At issue were rules set forth by the United Network for Organ Sharing, the non-profit that manages the national organ waiting list. It requires that the sickest children younger than 12 get priority for lungs donated from children younger than 12. Children age 12 and younger are eligible for lungs donated from 12- to 17-year-olds only after potential recipients between 12 and 17 have declined them. Lungs donated by adults are initially offered to all candidates older than 12.
Part of the rationale behind the “under 12 rule,” established in 2005 by the Organ Procurement Transplant Network, which is managed by UNOS, is that lungs from an adult would be too large for a child’s body. (There are no age-based cutoffs for transplanting organs other than lungs. The lobar structure of the liver makes it easier to reduce. Adult kidneys can be placed inside a child’s roomy abdominal cavity. But hearts must fit anatomical constraints.)
The age rule was also devised to compensate for a lack of good data for those under the age of 12. All lung transplant candidates over 12 are assigned a “lung allocation score” that reflects both the seriousness of a patient’s medical status and the likelihood of a successful operation. This score, in addition to blood type and the geographic distance between the candidate and the hospital with the lung donor, determines wait-list priority for receiving adult lungs. Patients under 12 are not assigned an LAS because the number of children in need of lung transplants is so small as to make statistical modeling difficult.
The devilish problem for children is that the donation numbers are badly skewed against them. Transplantable lungs from adults outnumber pediatric donations about fiftyfold. According to the OPTN, Sarah’s lung transplant from an adult donor is only the 11th of its kind since 1987, when national record-keeping on transplantation began.
As Sarah’s lungs began to fail, her frantic parents, Janet and Francis Murnaghan of Newtown Square, Pa., made public pleas to get her equal consideration with adults in need of lung transplants.
From a clinical standpoint, Sarah’s case sparked the question of whether the age rule is valid. After all, how great is the difference between a 10-year-old child and one who is one day past her 12th birthday? What’s more, Sarah’s physicians were confident that they could trim adult lungs to fit her chest cavity.
Against this backdrop, a fast-moving drama played out.
On Tuesday, June 4, lawmakers got involved, urging Health and Human Services Secretary Kathleen Sebelius, whose agency contracts with UNOS, to intervene. “I’m begging you,” Rep. Lou Barletta implored Sebelius, “she has three to five weeks to live.” Sebelius declined.
On Wednesday, June 5, District Court Judge Michael Baylson of Philadelphia overruled the secretary and blocked her from enforcing the age restrictions on children. This allowed Sarah to move to the front of the queue for adult lungs on the basis of the severity of her disease. Within a day, the mother of an 11-year-old Bronx boy at the same hospital and suffering from cystic fibrosis filed a lawsuit asking the judge to add him to the list. Javier Acosta, whose brother died of the disease in 2009 before he could receive a transplant, was also permitted to join the list of adults awaiting lungs.
On Monday, June 10, the executive committee of the OPTN ordered a yearlong review of wait-list guidelines for children in need of lungs. The network declined to suspend the age rule altogether—the physician experts tasked with reviewing the under-12 policy decided that there was no scientific evidence to justify a wholesale emergency change. But in the interim, it established a mechanism for doctors to request case-by-case exceptions for the roughly 30 other children younger than 12 who need lungs.
It was a happy ending for Sarah. Thanks to the judge’s ruling, the girl got a set of adult lungs about 18 months after being placed on the pediatric waiting list.
Sarah’s case is a classic illustration of the “rule of rescue.” Ethicist A.R. Jonsen coined the term to denote the imperative people feel to rescue identifiable individuals facing avoidable death. People may expend heroic efforts that either put others at risk or pose costs to society that could be more efficiently spent to prevent abstract deaths in the larger population. But the “baby in the well” is saved.
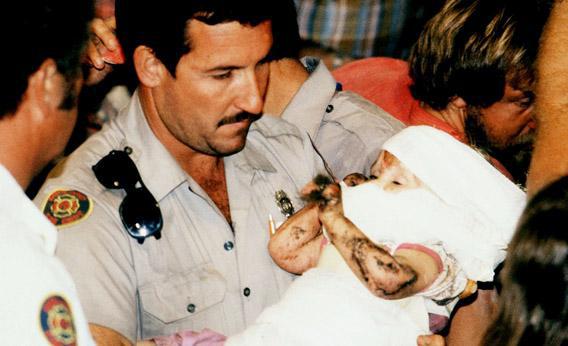
It was Jessica McClure, an 18-month-old girl who fell into a well in Midland, Texas, in 1987, who brought the rule of rescue intro millions of American living rooms. After 58 tense hours, emergency workers hoisted Jessica from the well; today she is a thriving mother of two. But Jessica’s case differed from Sarah’s: There was only one baby in a well. Saving her did not mean that another Jessica, in a well down the block, was left to suffocate.
And so we arrive at the most wrenching question of all: Did anyone die so that Sarah could live? When those adult lungs became available for the little girl, did another person, say a 21-year-old woman with cystic fibrosis, lose her claim on life?
That’s an agonizing question to pose. Yet it’s precisely the situation that our current transplant system, based on voluntary donation alone, forces everyone—patients, families, their doctors, politicians, and the HHS secretary—to confront.
When matters of fairness in health care come to the fore, the media reflexively turn to bioethicists. Daniel Wikler, a medical ethics expert at Harvard, took a dim view of special pleading. “If the distribution of organs becomes subject to the success of individual publicity campaigns, with organs going to those who hire the best PR firms and lawyers, who on the waiting list would remain confident that their priority would be decided on the merits?” David Magnus, a bioethicist at Stanford University, stressed how important it is for people who donate to have “faith in the system and that we have a fair system that also does a good job of marshaling and stewarding this incredibly scarce resource.”
Instead of settling for priority ratings and faith in a system that really does try to strike a utilitarian balance, the only real solution lies in increasing the organ supply. Nowhere in the modern medical universe, save for the world of transplantation, does the scarcity of the treatment dictate who will receive it.
In the end, the media attention that swirled around Sarah Murnaghan was eye-catching and effective—the rule of rescue was imposed. But her desperate need for an organ was not an exception. Her drama plays out every day as 18 people who can no longer survive the wait for precious kidneys, livers, hearts, and lungs succumb to the organ shortage.
Even if the rules for allocating lungs are permanently revised by the OPTN next year, the numbers of donated lungs will not likely change, and other unheralded “Sarahs” will perish needlessly.
Indeed, with annual donations falling far behind demand, we need to give people an incentive to donate. Sarah’s ordeal should force a re-examination of the 1984 National Organ Transplant Act, which makes giving something of material worth in exchange for an organ a felony punishable by up to five years in jail and/or a fine of up to $50,000.
A revision of NOTA would allow experimentation with incentives for donations. For organs such as lungs and hearts, the donor must be deceased. Perhaps an individual could agree to donate his organs at death in exchange for a burial benefit or a contribution to his or her estate when the time came. A third party, such as the government or a charity, could underwrite the cost of the benefit; the organ recipient would not pay for the lifesaving donation.
Kidneys can be donated by the living. Indeed, roughly half of all donors are friends or loved ones of recipients. To induce more strangers to save a life, compensation could again be provided by a third party and overseen by the government. Because bidding and private buying would not be permitted, available organs would be distributed to the next in line—not just to the wealthy. By providing in-kind rewards—such as a down payment on a house, a contribution to a retirement fund, or lifetime health insurance—the program would not be attractive to desperate people who might otherwise rush to donate on the promise of a large sum of instant cash.
Would prospective donors lie about their health to be eligible for compensation? This is not a major worry in the context of regulated exchanges, since they would have to undergo rigorous medical testing over several months, which is the current standard of care for altruistic donors. And donors or health care professionals could be made legally liable for any harm suffered by a patient as the result of receiving a diseased or substandard organ.
The state of Pennsylvania grasped the importance of rewarding donations years ago. In 1994 the late Gov. Robert P. Casey, who had received a heart and liver transplant a year earlier, signed a law that would enable a bereaved family of an organ donor to get a burial benefit of up to $3,000 paid by the state directly to the funeral home.
But then Pennsylvania health officials got cold feet. They feared that the law flouted NOTA. In the end they did not implement the funeral benefit.
Experts continue to debate the legality of a state or federal government rewarding donors or their families, but it’s hard to imagine that Congress truly intended that a widow in Harrisburg be punished for accepting a state-sponsored burial benefit.
Would such incentives work? There is good reason to be optimistic, but we need research to be sure. One thing that is inarguable is that our transplant system is a qualified failure. The organ shortage drove Sarah’s parents to plead for her life and to sue the federal government. A judge was pressed into overriding an expert panel of physicians. In the heat of it all, politicians tried to pressure a Cabinet secretary to decide who lives and who dies.
Compensating donors could spare us the heartbreak of rationing. Saving one person should not mean death for another.